A Guide to Operational Cost Reduction in Healthcare
Discover a practical roadmap for operational cost reduction in healthcare. Learn how AI, process redesign, and workforce optimization can lower expenses.
Cutting operational costs in healthcare isn't just a line item on a budget anymore—it's a matter of survival. We're talking about a strategic overhaul of technology and processes to fight back against soaring labor costs, dwindling reimbursements, and the relentless pressure of inflation. The old playbook of piecemeal cuts just won't work. To build a sustainable future, organizations need a fundamental shift in how they manage resources, and that's where powerful AI solutions come into play.
Why Healthcare Costs Are Spiraling Out of Control
If you're a healthcare leader, you know the feeling of being caught in a perfect storm. The demand for exceptional patient care never lets up, but the financial realities are getting tougher by the day. Traditional cost-cutting tactics—like across-the-board budget freezes or putting off equipment upgrades—are not only failing but often making things worse. They burn out staff, hurt the patient experience, and don't touch the real sources of inefficiency.
The problem isn't a lack of effort. It's that the operational models many health systems rely on are simply outdated. They're bogged down by manual administrative work, fragmented workflows, and a constant state of reactive problem-solving. These are the hidden leaks that silently drain margins, day in and day out.
It's Time to Move Past Temporary Fixes
Instead of just looking for things to trim, the real goal should be achieving true operational excellence. That means taking a hard look at core processes and being willing to rebuild them from the ground up. To really get at the root of the problem, you have to think systemically. It's about a comprehensive digital transformation in the healthcare industry that addresses these deep-seated issues head-on.
A strategic approach is the only way forward. It's about focusing on what truly matters:
- Process Redesign: Digging into your workflows to find and eliminate the bottlenecks and redundant steps that waste time and money.
- Workforce Optimization: Freeing up your skilled professionals to focus on high-value, patient-facing work instead of getting buried in administrative tasks.
- Strategic Sourcing: Using data to make smarter procurement decisions and cut down on supply chain waste.
- Technology Integration: Bringing in tools that automate the mundane and give your team the insights they need to make better decisions.
The global healthcare industry is under immense pressure, with medical trend rates expected to hit 10.0% in 2025. AI is poised to cut overall healthcare costs by $13 billion by 2025. On top of that, AI nursing assistants alone are projected to handle 20% of nurses' routine tasks, saving an estimated $20 billion a year. You can read more about these global medical trend rate projections.
AI Isn't Just a Tool—It's a Foundational Shift
Let's be clear: artificial intelligence isn't just another piece of software. It represents a completely new way to run healthcare operations. AI can automate repetitive work, predict resource demands before they become critical, and shine a light on inefficiencies you never knew you had. It allows for a proactive, intelligent approach to managing costs.
Investing in strategic Healthcare AI Services is no longer optional; it's a core requirement for building a resilient, financially sound organization. Think of this guide as your practical roadmap. We'll start by showing you how to pinpoint the high-impact areas ripe for improvement and build a rock-solid case for change.
Finding Your Highest-Impact AI Savings Opportunities
If you want to make a real dent in your operational costs, you can't just throw technology at every problem and hope for the best. The first, most critical step is figuring out exactly where new AI solutions will deliver the biggest financial payoff. A scattershot approach is a fast way to burn through your budget; a focused one builds momentum and proves its own ROI.
Before you even think about an investment, you need to take a hard, honest look at your current operations. This means going beyond surface-level complaints to uncover the root causes of inefficiency and financial drain. The good news is that most healthcare organizations are wrestling with the same core challenges, and that's often where the most fertile ground for AI-driven improvements lies.
This is the classic squeeze every healthcare leader is feeling today: costs are relentlessly climbing while reimbursements keep shrinking. It creates an urgent need for smarter, more efficient ways of working.
This reality is exactly why AI has become such a critical intervention. It turns these intense operational pressures into genuine opportunities for savings. To pinpoint where to start, I've found it's best to break operations down into four key areas.
The Four Core Domains for AI-Driven Savings
By digging into these specific domains, you’ll quickly start to see where your organization’s biggest pain points—and biggest opportunities—are.
-
Administrative Workflows: This is all the daily, thankless work that keeps the lights on but eats up an enormous amount of staff time. I’m talking about patient scheduling, manually keying in data from patient forms, and the endless back-and-forth of insurance pre-authorizations. Inefficiencies here don't just waste time; they create downstream headaches like appointment gaps and delayed care.
-
Clinical Operations: Here, we're looking at the direct delivery of patient care. Bottlenecks often show up as excessive overtime from inefficient staff allocation, long patient wait times in the ER, or expensive diagnostic equipment sitting idle. Streamlining these workflows has a direct impact on both your bottom line and patient experience.
-
Supply Chain Management: From surgical gloves to high-cost biologics, managing inventory is a tough balancing act. Overstocking ties up cash and leads to waste, especially with supplies that have an expiration date. Understocking is even worse—it can delay critical procedures. On top of that, hidden procurement and logistics costs can silently kill your margins.
-
Revenue Cycle Management (RCM): For most organizations, this is where the most significant financial leaks happen. The usual suspects are high claim denial rates from simple coding errors, painfully slow payment cycles from insurers, and an army of staff members chasing down unpaid bills.
From Inefficiencies to Actionable Insights
Spotting these problem areas is one thing, but connecting them to a tangible solution is the real challenge.
For instance, chronic scheduling logjams aren't just an annoyance; they represent real lost revenue and frustrated patients who might go elsewhere. All that manual data entry isn't just tedious; it's a primary source of the billing errors that lead to costly, time-consuming claim denials.
A detailed AI requirements analysis is what bridges the gap between knowing you have a problem and defining the right solution. It forces you to move beyond a vague "we need AI" to specifying exactly which processes to automate, what data you'll need, and what measurable outcomes to expect.
This kind of analysis often uncovers weak points you didn't even know were there. It grounds the conversation in data, helping you quantify the potential financial impact of closing your operational gaps. It's why we make this a core part of our AI strategy consulting—you have to aim before you fire.
Prioritizing AI Initiatives for Maximum Cost Reduction
To help connect the dots, we’ve found it useful to map common challenges directly to AI solutions and their potential impact. This helps executives quickly see which projects are likely to deliver the fastest or most substantial returns.
| Operational Area | Common Challenge | Targeted AI Solution | Potential Cost Impact |
|---|---|---|---|
| Administrative Workflows | Manual appointment scheduling & high no-show rates | AI-powered scheduling with predictive no-show alerts | High: Reduces staff overhead, optimizes provider utilization, cuts revenue loss |
| Clinical Operations | Inefficient staff rostering leading to overtime costs | Predictive staffing models based on patient census & acuity forecasts | High: Slashes overtime spending by 15-20%, improves staff-to-patient ratios |
| Supply Chain Management | Overstocking of perishable supplies & stockouts | AI-driven demand forecasting and inventory optimization | Medium: Reduces waste, lowers carrying costs, prevents procedure delays |
| Revenue Cycle Management | High claim denial rates due to coding errors | Natural Language Processing (NLP) for automated claim scrubbing | Very High: Drastically improves clean claim rate, accelerates cash flow, reduces A/R |
By looking at your operations through this lens, you can start building a business case for the initiatives that promise the biggest wins first.
Using Real-World Scenarios to Guide Your Strategy
Looking at real-world use cases makes the potential of AI concrete. For example, I worked with a hospital system where nurse burnout was a huge issue, driven largely by chaotic scheduling. They implemented an AI tool that predicts patient loads to optimize staff rosters. The result? They cut overtime costs by nearly 20% and saw a noticeable improvement in staff morale.
Another organization was getting hammered by claim denials. They brought in an AI platform to automatically scrub claims for common errors before submission. It completely changed their financial picture by improving their clean claim rate and speeding up cash flow.
Our expert team specializes in helping healthcare leaders navigate this discovery phase. We work with you to translate broad operational goals into a concrete, prioritized action plan. By focusing on the highest-impact opportunities first, you build a powerful case for change and show immediate, tangible value to your stakeholders.
Automating Administrative and Clinical Workflows
Administrative bloat and clunky clinical processes are two of the biggest, yet often overlooked, drains on a healthcare organization's resources. They are silent margin killers, driving up operational costs while frustrating both staff and patients. The good news? Tackling these areas with smart automation is one of the most direct paths to meaningful operational cost reduction in healthcare.
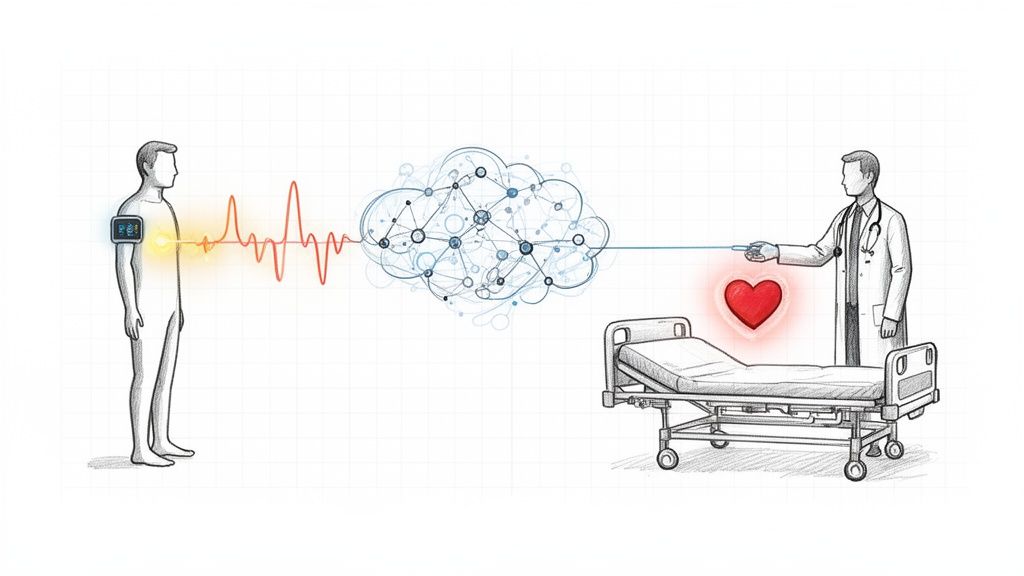
Think about the sheer volume of repetitive, manual tasks that happen every single day: patient scheduling, medical transcription, insurance verification, prior authorizations. Each one consumes countless hours from skilled professionals who should be focused on patient care. This is exactly where practical AI tools can make an immediate and significant impact.
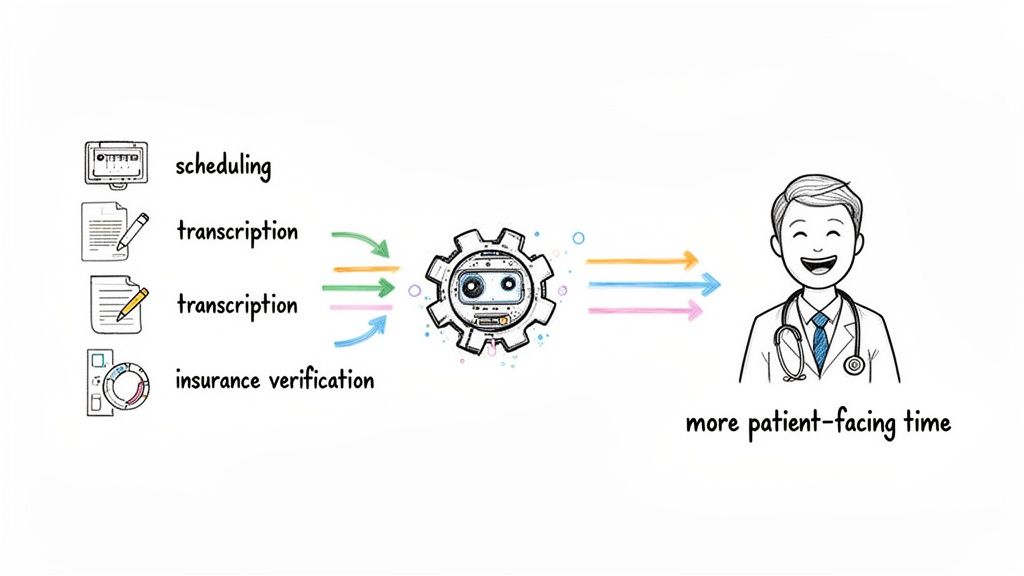
Automating these workflows isn't just about saving time. It's about reallocating your most valuable asset—your people—to where they can create the most value. By offloading this administrative burden, you not only cut labor costs but also boost staff morale, which is a critical advantage in today's tight labor market.
Taming Administrative Chaos with AI
Let's be honest, the financial pressures on providers are only getting worse. For instance, healthcare providers are bracing for a 2.83% cut in Medicare physician reimbursements in 2025. That squeeze is compounded by rising labor costs and medical inflation. With employers also staring down a 6.7% hike in their healthcare costs, automation has quickly moved from a "nice-to-have" to a strategic necessity.
Here are a few high-impact administrative areas where automation delivers quick and tangible wins:
- Intelligent Scheduling: Instead of playing phone tag, AI can optimize appointment slots, predict no-shows, and send automated reminders, minimizing those costly gaps in provider schedules.
- Automated Insurance Verification: Swapping manual phone calls for an automated system means AI can instantly verify patient eligibility and benefits, slashing claim denials before they even happen.
- Medical Transcription: AI-powered speech-to-text tools can accurately transcribe physician notes in real-time, freeing up clinicians from hours of documentation and keyboard time.
By automating these mundane but necessary tasks, a healthcare organization can reclaim thousands of staff hours every year. That time can be reinvested directly into patient care, complex case management, and other high-value activities that actually improve outcomes and patient satisfaction.
But it's not always a one-size-fits-all situation. Off-the-shelf software often struggles with the unique complexities of a specific healthcare system. This is where building custom internal tooling becomes a powerful strategy, allowing you to create solutions that integrate seamlessly with your existing EHR and solve the specific workflow bottlenecks that generic tools can't touch.
Optimizing Clinical Pathways for Efficiency
Beyond the back office, automation is also making huge waves in clinical operations. Efficient patient flow is directly tied to lower costs and better care, and this is an area where AI truly shines. It can analyze massive datasets to spot patterns and predict needs, turning what was once a chaotic clinical environment into a well-orchestrated system.
Imagine a system that analyzes historical patient data to predict ER admission volumes based on the time of day, the season, or even local community events. This allows for much smarter staff allocation, ensuring you have the right number of nurses and physicians on hand without getting hit with excessive overtime costs.
This predictive power also extends to optimizing clinical pathways for specific conditions. By analyzing treatment outcomes across thousands of patients, AI can help pinpoint the most effective and resource-efficient care protocols. This leads to a cascade of benefits:
- Shorter Patient Wait Times: Better resource allocation means patients move through the system faster.
- Improved Throughput: Optimized pathways allow you to treat more patients with the same resources.
- Standardized Quality of Care: Data-driven protocols ensure every patient receives the best possible care based on collective evidence.
This dual benefit—significant cost savings paired with a better experience for both staff and patients—is the real promise of automation. For a deeper look at redesigning these processes, explore these workflow automation strategies.
Optimizing Your Revenue Cycle and Supply Chain
Revenue leaks and inefficient supply chains are two of the biggest—and, frankly, most accepted—drains on a healthcare organization's finances. For years, we've treated them as complex, immovable problems. But that's changing. These are precisely the areas where a smart application of AI can deliver serious savings and give your financial health a major boost.
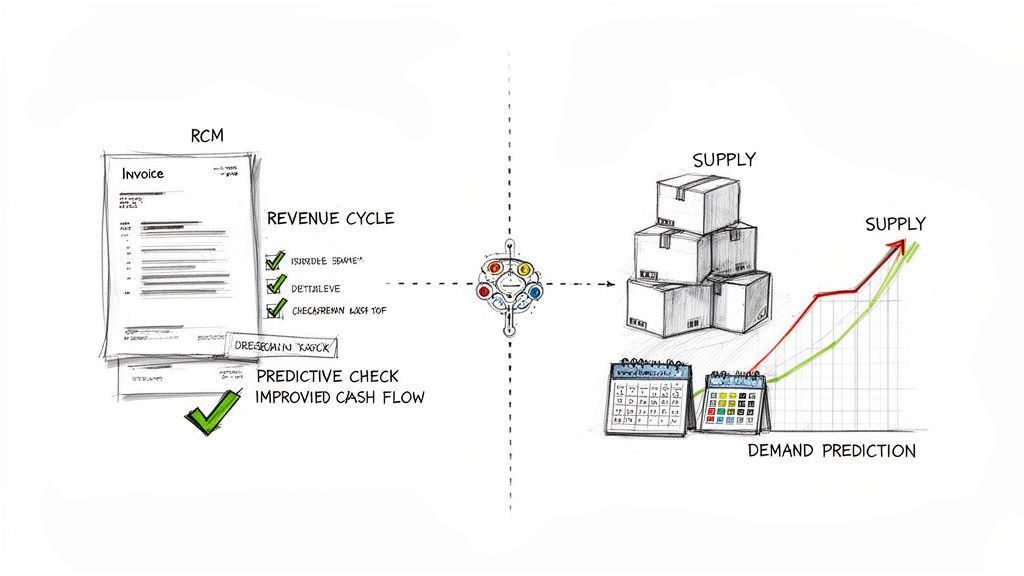
Think of your revenue cycle as a pipeline. Every single claim denial, coding error, or delayed payment is a leak. It’s not just a trickle, either. A recent analysis found that claim denials cost U.S. hospitals a staggering $262 billion every year, and the frustrating part is that many of them are entirely preventable. The same goes for supply chain waste, which quietly eats away at your margins through things like expired meds or over-ordered surgical kits.
This is where AI flips the script. It helps us move from constantly reacting to problems to proactively optimizing the entire system, turning these chronic cost centers into sources of real efficiency.
Fortifying the Revenue Cycle with AI
Before you can fix the leaks, you have to understand the plumbing. It’s worth getting grounded in the fundamentals of revenue cycle management in medical billing. With that foundation, AI's role becomes crystal clear. Imagine a system that analyzes mountains of your historical claims data to flag which submissions are likely to be denied before they ever leave your office.
That’s what this technology does. It gives your billing team a heads-up to correct errors in real-time, which can dramatically increase your clean claim rate. Instead of spending weeks chasing down denials on the back end, your staff can focus on getting it right the first time.
AI also brings some powerful automation to the table:
- Automated Medical Coding: Tools using Natural Language Processing (NLP) can scan a clinician's notes and suggest the right billing codes. This cuts down on the manual effort and human error that so often lead to rejections.
- Smarter Patient Billing: AI can automate payment reminders, tailor the communication style to a patient's history, and even offer flexible payment plans. This gets cash in the door faster and lightens the load on your collections team.
The impact here is real and direct. By plugging revenue leaks at the source, AI ensures you get paid fully and promptly for the care you deliver. It's a straight line to a healthier bottom line.
Creating an Intelligent Supply Chain
When it comes to the supply chain, AI helps us move from educated guesswork to data-driven precision. For too long, inventory management has relied on historical averages, trapping us in a cycle of either having too much on the shelves or not enough. Predictive analytics breaks that cycle for good.
AI models can look at patterns in patient admissions, surgical schedules, and even things like local flu season trends to forecast demand for specific supplies with incredible accuracy. You end up ordering what you need, right when you need it.
This smarter approach pays off in a few key ways:
- Less Waste: AI forecasting is a game-changer for perishable items like pharmaceuticals or lab reagents, preventing them from expiring on the shelf.
- Optimized Ordering: The system can automatically trigger purchase orders when stock hits a dynamically calculated level, freeing up your procurement team to focus on more strategic work.
- Stronger Vendor Negotiations: When you walk into a negotiation armed with precise demand data, you're in a much better position to secure favorable pricing from suppliers based on predictable purchasing volumes.
Many organizations I've worked with find that standard software just doesn't quite fit their unique RCM or supply chain needs. This is where building a custom solution can be a huge advantage. An integrated platform designed for your specific workflows creates a seamless system that maximizes efficiency, instead of forcing your teams to work around a generic tool’s limitations.
As you start thinking about these financial wins, checking out a Financial Insights Dashboard can give you a clear picture of your progress. You can see an example of what that looks like here: https://www.ekipa.ai/products/financial-insights-dashboard.
Building a Business Case That Wins Executive Buy-In
Even the most brilliant AI initiative can die on the vine without executive approval. Getting that crucial green light isn't about having a good idea; it's about building a bulletproof business case that speaks the language of the C-suite—finance, risk, and return. Your proposal has to answer one fundamental question, loud and clear: "How will this investment make our organization stronger?"
A compelling justification has to move beyond the cool tech features and focus squarely on business outcomes. It’s all about translating the potential of AI solutions into the tangible financial metrics that get a CFO's attention. That means you have to quantify projected cost savings, forecast real efficiency gains, and estimate potential revenue improvements in a way that’s both credible and compelling.
Quantifying the Return on Investment
Let's be direct: the heart of your business case is the Return on Investment (ROI) analysis. Vague promises of "improved efficiency" simply won't cut it in the boardroom. You need to draw a straight line from your proposed AI project to specific, measurable financial gains.
So, where do you start? Begin by pinpointing the key performance indicators (KPIs) the initiative will actually move. Think of these as the vital signs of your operational health; they provide the hard data you need to build a strong financial model.
Here are a few essential KPIs I always look at when evaluating cost-reduction opportunities in healthcare:
- Cost-Per-Claim: What's the total expense to process a single insurance claim? AI can hammer this number down by automating coding and slashing manual rework.
- Patient Wait Times: Long waits are more than just a patient satisfaction issue. They often signal workflow bottlenecks and poor resource allocation, which are incredibly expensive.
- Staff Overtime Hours: If you see consistently high overtime, that’s a flashing red light for staffing inefficiencies. Predictive analytics can get you ahead of the curve here.
- Supply Spoilage Rates: For things like pharmaceuticals or biologics, waste is a killer. AI-driven inventory management can dramatically cut those losses.
- Claim Denial Rate: This is a direct measure of revenue just walking out the door. Trimming this by even a few percentage points can lead to a massive financial windfall.
Once you’ve identified your KPIs, you can start building a financial forecast. For instance, say your average claim denial rate is 10%. If an AI tool can realistically knock that down to 7%, you can calculate the direct dollar increase in collected revenue. That's a hard number you can confidently take to any executive.
Start Small, Prove Value with a Pilot Project
Trying to sell a massive, organization-wide AI overhaul right out of the gate is usually a recipe for rejection. The perceived risk and cost are just too high. A much smarter approach is to start with a focused pilot project.
A pilot lets you demonstrate real value in a controlled environment. It minimizes the upfront investment and, more importantly, builds the momentum you need for broader adoption down the road.
Key Takeaway: A successful pilot project is your best internal marketing tool. It generates real data, creates internal champions, and proves the technology's value, making it much easier to secure funding for scaling the initiative.
This strategy fits perfectly with an agile AI Product Development Workflow, allowing you to test, learn, and iterate quickly. My advice? Pick a use case with a high probability of a quick win. Think about automating prior authorizations in a single department or optimizing the schedule for one clinical unit.
Crafting a Data-Backed Proposal
This is where getting some expert guidance can be a game-changer. An experienced AI strategy consulting service can help you navigate this whole process, making sure your business case is built on solid data and realistic projections. They bring an essential outside perspective, helping you sidestep internal biases and benchmark your potential gains against what others in the industry are seeing.
Ultimately, the goal is to produce a Custom AI Strategy report. This document becomes your formal proposal, meticulously linking the technology investment to core business objectives. It needs to clearly articulate the problem, the proposed AI solution, the pilot project plan, the key metrics for success, and, of course, a detailed financial analysis.
When you walk into that meeting with a business case that is data-driven, focused, and directly tied to improving the bottom line, you change the conversation from "Can we afford this?" to "How quickly can we get started?" It's a strategic approach that not only wins buy-in but sets the entire project up for a successful and impactful implementation.
From Plan to Reality: Implementing Your AI Strategy and Dodging Common Pitfalls
A great strategy on paper doesn't automatically translate into real-world results. Getting from a compelling business case to a successful implementation is where the real work begins. To achieve meaningful operational cost reduction in healthcare with AI, you need a realistic roadmap that accounts for both the technology and, just as importantly, the people who will use it.
This journey starts with the human side of the equation. Let's be honest—introducing new technology can stir up skepticism, especially among staff who are already stretched thin. The secret is to frame these new AI tools for business not as replacements, but as powerful partners. Their job is to take over the tedious, administrative burdens and free up your skilled professionals to focus on what matters most: patient care.
Bringing your clinical and administrative teams into the conversation early is non-negotiable. They need a seat at the table during the selection and rollout process. Why? Because they know the real-world problems that need solving. This kind of collaboration, as we explored in our AI adoption guide, is how you build a network of internal champions who will drive adoption from the ground up.
Sidestepping the Usual Implementation Roadblocks
Once you've got your people on board, it's time to tackle the practical challenges. I've seen more than a few promising AI projects get derailed by predictable, avoidable issues. Staying ahead of them is key.
- Data, Data, Data: An AI model is completely dependent on the quality of its data. Pulling clean, consistent information from siloed systems—your EHR, billing platforms, supply chain software—is often the biggest technical lift. You need a solid plan for data cleansing and harmonization before you even start.
- Compliance is Not Optional: Patient data is sacrosanct. Any AI tool you bring in must be bulletproof when it comes to HIPAA and other privacy regulations. This means ironclad encryption, strict access controls, and a vendor who can prove their security bona fides.
- Picking the Right Partner: Choosing your technology vendor is a critical decision. Be wary of those who make grand promises but lack specific, demonstrable real-world use cases. A good partner will be completely transparent about their tech, their security, and how they integrate. They might even offer custom healthcare software development to ensure the tool fits your workflow, not the other way around.
Start Small, Scale Smart: The Phased Rollout
It can be tempting to go for a big-bang, system-wide launch, but that’s rarely the best approach. A phased rollout, starting with the focused pilot project you already defined, is almost always the smarter play. This strategy lets you minimize risk, iron out the wrinkles in a controlled setting, and—most importantly—generate quick wins that build momentum.
Your pilot project is your best internal marketing tool. A successful pilot delivers clear ROI and turns even the biggest skeptics into supporters, which makes scaling up across the organization infinitely easier.
Achieving sustainable cost savings is a marathon, not a sprint. Our Healthcare AI Services are built to guide you through every stage of this journey, from initial brainstorming to full-scale implementation. If you're ready to build a practical roadmap for your organization, let's connect with our expert team.
Answering Your Top Questions
When I talk with healthcare leaders about bringing AI into their cost-reduction strategy, a few key questions always come up. Let's tackle them head-on.
Where on Earth Do We Start with AI for Cost Reduction?
The best way to begin is by doing a sharp, focused opportunity assessment. Don't get distracted by the latest shiny AI tool. Instead, look at your own operations and pinpoint the 3-5 areas where you're feeling the most financial pain.
Often, this means looking at revenue cycle management, grappling with staff scheduling, or getting buried under administrative tasks. A dedicated AI strategy consulting engagement can cut through the noise, analyzing your specific workflows and data to find the use cases with the fastest and highest return. It's all about securing a quick, impactful win right out of the gate.
How Do We Get Approval for the Upfront Investment?
You need to build a rock-solid business case centered on near-term ROI. Forget about proposing a massive, system-wide overhaul. Instead, pitch a tightly focused pilot project.
For instance, think about what happens if you implement an AI tool that reduces claim denials. Even a modest 15% reduction can unlock a significant amount of revenue—often more than enough to cover the initial cost of the technology. A Custom AI Strategy report is perfect for this, as it helps you model these financial projections and present a clear, data-backed argument to the board.
How Can We Implement This Without Overwhelming Our Staff?
This is a critical point. A successful AI rollout should feel like a relief to your team, not another burden.
- Frame AI as a "digital assistant." It’s not here to replace people, but to handle the tedious, repetitive work like data entry and paperwork. This frees up your clinical experts to focus on what they do best: patient care.
- Bring your people in early. Involve clinical and administrative staff in the selection process from the beginning. If they help choose the tool, you can be sure it solves a problem they actually have.
- Roll it out in phases. A gradual implementation, paired with solid training, is the key to smooth adoption. When your team sees the immediate benefits for themselves, buy-in happens naturally.
When you take this approach, AI stops being another new system to learn and becomes a valued partner in their daily work. For more on navigating these changes, our AI adoption guide has practical steps for a smooth transition. Or, if you'd like to talk through a plan tailored to your organization, feel free to connect with our expert team.
Frequently Asked Questions (FAQ)
What are the main drivers of rising operational costs in healthcare?
The primary drivers include escalating labor costs for skilled professionals, decreasing reimbursement rates from insurers, high administrative overhead from manual processes, and supply chain inefficiencies. These factors create a financial squeeze that requires strategic, technology-driven solutions for sustainable cost management.
Can AI really help with operational cost reduction in healthcare?
Absolutely. AI can automate repetitive administrative tasks, optimize staff scheduling to reduce overtime, predict supply needs to minimize waste, and streamline the revenue cycle to decrease claim denials. By improving efficiency and reducing manual errors, AI directly lowers operational expenditures while often improving the quality of care.
How do you measure the ROI of an AI implementation for cost reduction?
ROI is measured by tracking key performance indicators (KPIs) before and after implementation. Key metrics include the claim denial rate, staff overtime hours, cost-per-claim, supply spoilage rates, and patient wait times. Quantifying improvements in these areas allows you to calculate the direct financial savings and revenue gains generated by the AI investment.
What is the biggest challenge when implementing AI in a healthcare setting?
The most common challenge is data integration and quality. Healthcare data is often stored in disparate, siloed systems (EHR, billing, etc.). Ensuring that AI tools have access to clean, standardized, and comprehensive data is a critical first step. Another significant challenge is managing change and ensuring staff buy-in through clear communication and training.