Healthcare Change Management Strategy for Digital Transformation
Discover a healthcare change management strategy that accelerates digital transformation with practical steps for AI adoption, cost control, and lasting impact.

A solid healthcare change management strategy is more than just a project plan. It's a structured, human-centered approach that carefully guides people, teams, and entire organizations from where they are today to where they need to be tomorrow. This isn't about just checking boxes on a project timeline; it's about navigating the human side of change to get real buy-in, minimize resistance, and make sure new processes and technologies actually deliver on their promises. From implementing new healthcare software solutions to overhauling patient care workflows, a robust strategy is the difference between success and failure.
Why Old Change Management Fails in Modern Healthcare
Let’s be honest—the old top-down change management playbook is broken, especially in a field as dynamic as healthcare. Traditional, rigid methods simply crumble under the pressure of digital transformation, soaring operational costs, and the constant influx of new technologies. Healthcare is just moving too fast for yesterday's slow, hierarchical approval chains.
Today’s complex healthcare ecosystem demands a strategy that is agile, deeply human-centric, and backed by solid data. This isn't a "nice-to-have" anymore; it's a fundamental requirement for survival and growth.
The Blistering Pace of Digital Transformation
The push for digital adoption in healthcare is relentless. It's no surprise that accelerated digital transformation is the top priority for global health systems. In fact, a staggering 90% of C-suite executives expect its adoption to speed up significantly.
This urgency makes sense when you consider how far behind some organizations are—many still rely on fax machines. A recent survey highlighted that 70% of executives see digital platform investments as essential, which really drives home the need for change strategies that can help them leapfrog legacy issues. You can read more on these 2025 healthcare executive outlooks on deloitte.com to get a sense of the scale of this shift.
This rapid evolution makes traditional change models, with their slow, linear phases, completely obsolete. A modern approach has to be iterative and adaptive, ready to pivot based on new information and real-time feedback.
Key Takeaway: The friction isn't just about the technology itself; it's about people and processes. A top-down mandate to "use the new system" almost always fails because it completely ignores the deeply ingrained workflows of clinicians and administrators who are already stretched thin.
Disconnected Workflows and Communication Breakdowns
Another critical failure point is communication. Old strategies were notorious for broadcasting changes from the top down, leaving no room for feedback from the frontline staff who are most affected. This one-way street is a recipe for resistance and misunderstanding. To see how this plays out, it's insightful to understand why healthcare organizations are replacing WhatsApp with more secure, professional platforms to manage change effectively.
This shift underscores the need for dedicated, two-way communication channels built directly into any change initiative. For any transformation to stick, it needs a comprehensive approach supported by robust software and deep expertise. We’ve seen firsthand how integrated Healthcare AI Services can tackle these modern challenges by automating communication and providing data-driven insights that were previously out of reach.
The goal is to create a unified system where clinicians, administrators, and IT are all working together, not in their own silos. Without that cohesion, even the most promising tech will fail to gain traction, leading to wasted resources and deeply frustrated teams. A new approach isn't just better—it's essential.
Legacy vs Modern Change Management in Healthcare
To really grasp the shift, it's helpful to see the old and new approaches side-by-side. The differences are stark and show why modern strategies are built for the realities of today's healthcare environment.
| Characteristic | Legacy Approach (Ineffective) | Modern Strategy (Effective) |
|---|---|---|
| Pacing | Slow, linear, and phased. | Fast, iterative, and adaptive. |
| Communication | Top-down, one-way broadcast. | Two-way, continuous feedback loop. |
| Focus | Project-centric (implementation). | People-centric (adoption and value). |
| Technology | An endpoint or goal. | An enabler integrated into workflows. |
| Decision-Making | Hierarchical, siloed approvals. | Data-driven, collaborative, and agile. |
| Training | One-time event before go-live. | Ongoing, on-demand, and personalized. |
| Success Metric | "On-time and on-budget." | Adoption rates and business outcomes. |
Ultimately, clinging to legacy methods is like trying to navigate a superhighway with a horse and buggy. Modern change management provides the engine and the GPS needed to succeed in a complex, fast-moving industry.
Crafting Your Framework for Change That Actually Sticks
Let's be honest: most change management strategies in healthcare feel like a rigid, top-down checklist. But real, lasting change doesn’t come from ticking boxes. It comes from building a dynamic, adaptive framework that can handle the pressures of a complex clinical setting. You need a structure that can bend without breaking.
To get from a good idea to a successfully adopted reality, we’ve found that a five-part framework is the most effective approach:
- Vision & Assessment
- Stakeholder Governance
- Strategic Communication
- Agile Implementation
- Continuous Measurement
This structure isn't just a sequence of steps; it's a way to build momentum, deliver value quickly, and keep people at the very center of the process. It’s about moving away from the old, slow, and linear methods that just don't work anymore.
The difference between the old way and this modern approach is stark.

As you can see, legacy models get bogged down in bureaucratic phases. A modern strategy, on the other hand, is all about continuous feedback and adaptation. It’s a loop, not a straight line.
Vision and Assessment: Your Starting Block
Every meaningful change starts with a clear, compelling vision. This is more than just a goal; it's the why. Why does this matter to our patients? To our clinicians? A vague target like "improve efficiency" is basically useless. Get specific. A vision like "reduce patient intake time by 25% using AI-powered automation" gives everyone a concrete destination and a reason to care.
Right alongside that vision, you need a brutally honest assessment of your organization's readiness. This isn't just a technical check-up. While a thorough AI requirements analysis is critical, you also have to gauge the cultural climate, anticipate workflow disruptions, and map out your current digital capabilities. Skipping this step is like building a house on a shaky foundation—it’s bound to crumble.
Stakeholder Governance: Figuring Out Who Leads the Charge
Big changes need dedicated leadership, and I don't just mean a directive from the C-suite. This is where stakeholder governance comes in. It’s about assembling a cross-functional change committee that has real teeth and represents a microcosm of your organization.
This group absolutely must include:
- Clinical Champions: Respected physicians or nurses who get the realities of the frontline and can rally their peers.
- Administrative Leaders: People from finance, HR, and operations who know how to cut through red tape and align the change with business goals.
- IT and Data Specialists: The technical gurus who make sure the new systems are secure, integrated, and actually work.
- Frontline Staff Representatives: The nurses, medical assistants, and billing coordinators who can give you priceless, on-the-ground feedback about how the change is really affecting their day-to-day work.
Without this coalition, even the best-laid plans will feel disconnected from the people they’re supposed to help, leading to dismal adoption rates and wasted money.
Strategic Communication and Agile Implementation
With your vision set and your team in place, it’s time to execute. Communication is the lifeblood of this process. It has to be strategic—delivering the right message to the right people at the right time. Ditch the mass emails. Create targeted messages that speak directly to each group's concerns and answer that all-important question: "What's in it for me?"
One of the biggest mistakes I see is treating implementation as a single, terrifying "go-live" event. A much smarter strategy is to take an agile approach, breaking the project into smaller, digestible phases.
This method, which mirrors our own AI Product Development Workflow, is built for rapid feedback and constant improvement. Start with a pilot program involving a small, enthusiastic group. This lets you iron out the kinks, create early wins, and build powerful success stories that create a groundswell of support for the wider rollout.
Continuous Measurement and Adaptation
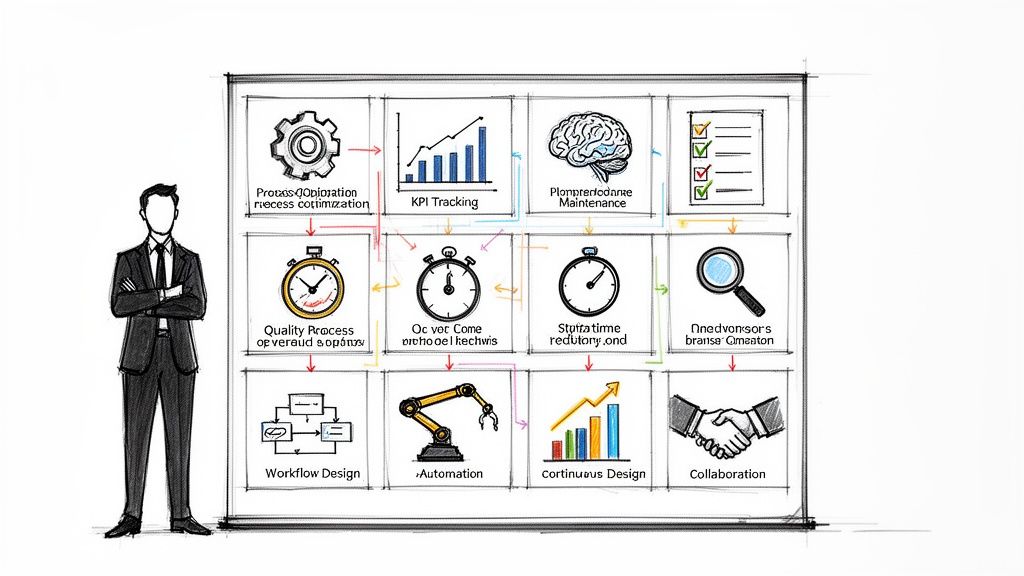
So, how do you know if any of this is actually working? That’s the final pillar: continuous measurement. You need to track your progress against clear, predefined metrics. And I’m not just talking about technical KPIs like system uptime.
True success is a blend of hard numbers and human feedback:
- Adoption Rates: Are people actually using the new tool or process?
- Time Savings: Are workflows getting faster? By how much?
- Error Reduction: Is the change making care safer and more accurate?
- Staff Satisfaction: How do your people feel about this new way of working?
This data isn't just for a final report; it's a vital feedback loop that lets you tweak and adapt your strategy in real-time. Pulling together a Custom AI Strategy report from the very beginning can establish this entire framework, ensuring your change initiative is built on a solid, measurable, and adaptive base from day one.
Navigating the Human Side of Digital Transformation
Let's be honest: technology is just the tool. It's the people who make or break any real transformation. In healthcare, that truth is magnified tenfold. A successful healthcare change management strategy has to go far beyond project plans and deployment schedules. It must dive deep into the human side of change—tackling everything from physician burnout to the very real resistance from administrative staff.

Guiding people through this transition isn’t about checklists. It's about building trust, creating a sense of psychological safety, and earning genuine buy-in. The first step is acknowledging that resistance isn't just stubbornness; it's often a symptom of very valid concerns.
Identifying and Empowering Your Change Champions
Every healthcare organization has them. They're the respected clinicians and administrators who others naturally turn to for advice. These individuals are your most powerful allies, and getting them on board is one of the single most effective ways to build momentum from the ground up.
Think of these "change champions" as the crucial bridge between leadership's vision and the frontline's reality. They can translate high-level strategic goals into practical benefits that actually make sense in a day-to-day workflow. When they adopt a new process and talk about it positively, they provide the social proof their colleagues need to see that the new way isn't just possible, but better.
To really empower them, you need to do more than just give them a title:
- Involve them early. Don't wait until the decisions are made. Bring them into the planning process for their insights—it will make the entire strategy stronger and more realistic.
- Give them a real voice. This is critical. Make sure their feedback isn't just heard, but visibly acted upon. This proves it’s not just another top-down mandate.
- Equip them for success. They'll need the right training, resources, and a direct line to project leaders to get answers for their colleagues.
Creating a Culture of Psychological Safety
Change is unsettling, period. In high-stakes clinical environments, staff need to feel safe enough to voice concerns, admit they're struggling with a new system, or point out a flaw without fearing they'll be judged or punished. That's the core of psychological safety.
Without it, you get surface-level compliance, not true adoption. People will nod along in meetings and then immediately revert to their old habits once they're back at their desk or in an exam room.
Key Takeaway: You can't build a resilient organization on a foundation of fear. Psychological safety is what unlocks the honest—and sometimes difficult—conversations needed to solve the real-world problems that always pop up during a major transformation.
Fostering this environment means leaders must actively ask for dissenting opinions, treat problems as opportunities to get better, and be transparent about both the challenges and the wins.
Answering the “What’s in It for Me?” Question
Effective communication is the engine of change, and it has to answer the one question on every single person's mind: "What's in it for me?" A generic, one-size-fits-all email from the top just won't cut it. You have to speak directly to the specific pains and motivations of each role in your organization.
Imagine you're introducing a new AI-powered automation tool to a skeptical billing department. A message focused on corporate ROI is going to be met with eye-rolls and a healthy dose of fear about job security.
Instead, frame the technology as a solution to their daily headaches:
- For the Billing Specialist: "This new tool will take over the tedious work of chasing down prior authorizations. That means you can focus your expertise on the complex cases where you really make a difference."
- For the Department Manager: "This will drastically cut our denial rates, helping your team hit its targets and making those month-end reports a lot less stressful."
This kind of role-specific messaging turns the change from a threat into an empowering tool. To really nail this communication and connect it to your bigger goals, you might find our interactive AI Strategy and Innovation Workshop helpful. It’s where we help teams craft these exact value propositions. This targeted approach, built on empathy for daily workflows, is what turns resistance into advocacy and makes innovation feel like a shared victory, not just another burden.
Putting Technology and AI to Work—With a Human Touch
This is the moment of truth. You've got a strategy on paper, but now it's time to bring it to life on the hospital floor. A successful healthcare change management strategy isn’t just about flicking a switch on new software; it's about weaving technology—especially sophisticated AI tools—into the fabric of daily patient care without missing a beat.
The real goal is to make any new tool feel like a natural extension of a clinician's expertise, not another soul-crushing login screen or a clunky interface that adds to their workload.

This requires a people-first approach at every turn. Forget those generic, one-size-fits-all training sessions that feel more like a software lecture. Instead, your training needs to be hyper-specific to the person's role and show them exactly how the new tool fits into their existing workflow. You have to answer that all-important "what's in it for me?" question right out of the gate.
Start Small, Win Big: The Power of a Pilot Program
One of the best moves you can make for a smooth rollout is to start small. A pilot program lets you introduce new technology to a hand-picked group of early adopters—the people who are genuinely excited about innovation. This isn't just a test run; it's your chance to cultivate powerful success stories that build momentum and help win over the skeptics.
This controlled launch allows you to:
- Find and fix workflow snags before they impact the entire organization.
- Collect honest, on-the-ground feedback to fine-tune your training and support.
- Create internal champions who can share their positive experiences with colleagues. A recommendation from a trusted peer is always more powerful than a memo from leadership.
When you secure a small win first, you build a foundation of confidence and proof. The broader rollout then feels less like a risky gamble and more like a smart, logical next step. You can see how we apply this phased approach on our Implementation Support page.
Design Training That Actually Sticks
Great training isn't about teaching people which buttons to click. It’s about showing them how a tool solves a real, everyday problem they face. The most effective training is built around scenarios that your staff will instantly recognize from their own demanding schedules.
For instance, instead of a general training on a new electronic health record (EHR) feature, get specific:
- For Nurses: "How to Cut Charting Time by 15 Minutes Per Shift with This New Feature."
- For Physicians: "Get Lab Results Faster with the Integrated Diagnostics Dashboard."
- For Billing Staff: "Automate Prior Authorization to Slash Denials."
This kind of targeted training makes the value proposition crystal clear from the start, which is key for both engagement and long-term adoption.
A Real-World Pressure Point: The current financial squeeze on healthcare is making smart tech adoption more critical than ever. With 82% of healthcare CFOs reporting a spike in payer denials, two-thirds of organizations are now increasing their AI spending, particularly for revenue cycle management. This is where AI-driven analytics can help predict and prevent denials while upskilling staff to take on new AI-auditing roles.
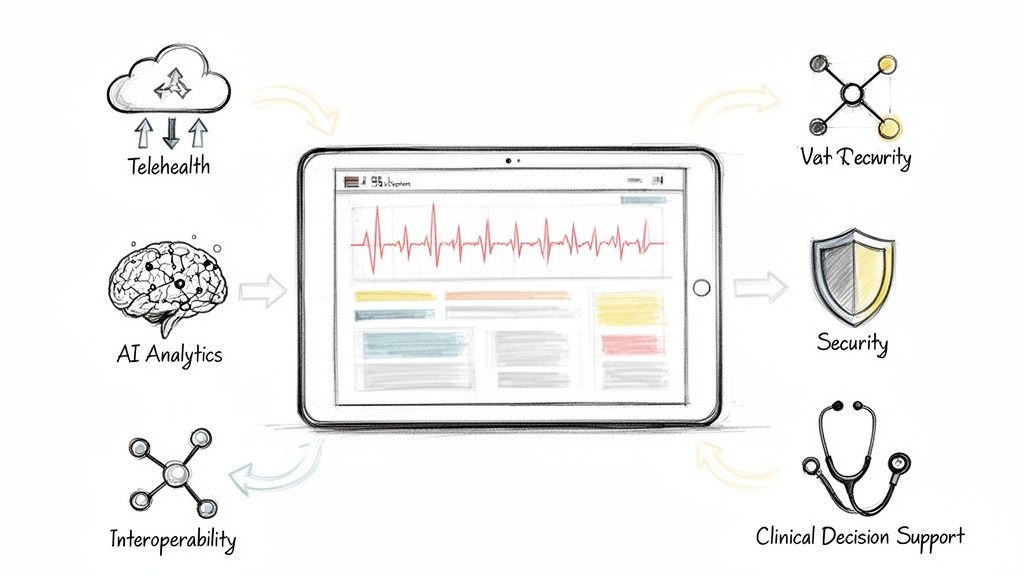
Using Smart Tools to Support the Change
To manage a change of this scale, the right internal tooling can make all the difference. Think about creating a centralized knowledge base with quick video tutorials, a dedicated Slack or Teams channel for instant support, or simple dashboards to track adoption rates.
These resources streamline the rollout and provide a safety net for your team long after the initial training sessions are over. And remember, as you bring in new technology, robust healthcare cybersecurity is non-negotiable to protect sensitive patient data.
By pairing a people-first mindset with smart pilots and supportive tooling, you can ensure that technology truly empowers your staff to deliver better care, instead of becoming just another source of frustration.
How to Tell if Your Change Initiative is Actually Working
So, you’ve launched the new system. The training is done. Now what? How do you know if all that effort is paying off? You can't just cross your fingers and hope for the best. A successful healthcare change management strategy needs proof, not just anecdotes.
This is where you build a measurement framework that shows the real value of the change. It's about getting past simple vanity metrics and zeroing in on the Key Performance Indicators (KPIs) that actually mean something in a busy clinic or hospital. The goal here is to create a constant flow of feedback so you can tweak your approach, celebrate real wins, and show stakeholders a tangible return on their investment.
Building Your Measurement Framework
A solid framework isn't just about the numbers. It’s a blend of hard, quantitative data and the qualitative feedback that tells you the human side of the story. This mix gives you the full picture—how the change impacts both your bottom line and the people doing the work.
You’ll want to track metrics across a few critical areas:
- Technology Adoption: This is more than just counting logins. You need to know if people are using the new tools in a meaningful way. Are physicians actually using the advanced features in the new EHR? Is the revenue cycle team using the new automation software to its full potential? A dip in adoption is often the first red flag that your strategy needs a second look.
- Operational Efficiency: This is where you connect the change to day-to-day workflows. You're looking for things like time saved on specific tasks, a drop in administrative mistakes, or faster patient processing times. For instance, a well-executed E-prescribing rollout should directly lead to fewer hours spent on the phone with pharmacies.
- Clinical and Patient Outcomes: At the end of the day, any change in healthcare has to improve care. You should be measuring things like fewer medication errors, better adherence to clinical protocols, and, of course, patient satisfaction scores.
- Staff Experience: Don't forget the people on the front lines. This is the qualitative side of your measurement. Use quick pulse surveys, small focus groups, and even casual one-on-one conversations to check in on staff satisfaction, perceived stress, and overall morale. High burnout can quietly sabotage even the best technology.
A lot of people treat measurement like it's the final step. It's not a report card you get at the end; it's your GPS for the entire journey. Constant measurement gives you the data you need to make smart adjustments in real time.
Creating Dashboards That People Actually Use
The data you're collecting is worthless if it's stuck in a spreadsheet nobody can understand. The trick is to build simple, visual dashboards that give leaders and key stakeholders a quick, clear view of how things are going. These dashboards are meant to provide clarity, not create more work.
A good dashboard might show:
- A line graph tracking weekly active users of the new software.
- A bar chart showing the month-over-month reduction in denied claims.
- A simple "stoplight" chart (red, yellow, green) that summarizes staff sentiment by department.
This kind of visual reporting keeps everyone on the same page and focused on the metrics that drive success, making it far easier to justify the project and keep the momentum going.
Making the Change Stick for the Long Haul
Getting to launch day is a milestone, not the finish line. As we've explored in our AI adoption guide, real success comes from ongoing support, positive reinforcement, and a culture of continuous improvement. You know adoption is sustainable when the new way of doing things becomes part of your organization's DNA.
Your measurement framework is your best tool for this. By tracking your KPIs over the long term, you can spot opportunities for more training, find ways to optimize workflows, and even identify the next logical technology upgrade. This turns a one-off project into a cycle of lasting improvement.
This ongoing process of measuring and refining is central to our AI strategy consulting philosophy. We focus on helping organizations not just implement change, but build the internal muscle to sustain it for years to come. Because a successful change is one that sticks, and that only happens when you measure what matters and never stop listening to your people. Feel free to connect with our expert team to see how we build these kinds of sustainable frameworks.
Where Do You Go From Here?
Think of your change management strategy not as a project with a start and end date, but as a new muscle your organization needs to build. It’s about creating a culture of resilience and continuous improvement, rather than just bracing for the next big disruption. This whole journey rests on the foundations we’ve covered: a vision that people can rally behind, a team that feels empowered, a smart and flexible approach to implementation, and a commitment to measuring what matters.
Taking that first step from a detailed plan to real-world action can feel like the hardest part. It's completely normal to feel a bit overwhelmed. But you don't have to figure it all out in a vacuum.
Whether you're just looking for a solid framework to get started—something like our AI Strategy consulting tool can help—or you need a team to roll up their sleeves alongside you, the right support changes everything. We’ve always believed that technology is a tool meant to help people, and that's especially true in healthcare.
Ultimately, all the strategies and tools in the world are only as good as the people who bring them to life. If you’re ready to have a real conversation about what’s next for your organization, our team of experts is here to listen.
Let’s build a more adaptive, resilient, and human-focused future for healthcare. Together.
FAQs: Common Questions on Healthcare Change Management
When you're knee-deep in planning a major change, questions are going to pop up. It’s part of the process. Here are some of the most common ones I hear from leaders and my take on how to tackle them.
What’s the single biggest mistake you see in healthcare change management?
Easy. Forgetting who does the actual work. Too many strategies look great on a PowerPoint slide but fall apart on the hospital floor because they were dreamed up in a boardroom without a single doctor or nurse in the room. If you don't co-create the change with your clinical frontline, it's doomed. You have to bring them in from the very beginning. Listen to their real-world workflow issues and make it crystal clear how this new process or technology will genuinely make their demanding jobs easier and directly improve patient outcomes—not just boost a metric on a spreadsheet.
How do we actually measure the ROI of all this work?
Thinking about the return on investment for change management requires looking beyond just the hard numbers. A true picture combines both the quantitative and the qualitative.
- The Quantitative Side: This is the stuff you can count. Look at tech adoption rates, time saved on administrative tasks, drops in error rates, and any direct cost savings. These are your hard metrics that showcase efficiency gains from solutions like AI Automation as a Service.
- The Qualitative Side: This is about the human impact. Track things like staff satisfaction scores, physician burnout levels, and feedback from patient experience surveys.
When you put both together, you don't just see a financial return; you see a cultural one, which is arguably more valuable in the long run.
Any advice for dealing with resistance from seasoned staff or physicians?
Resistance is rarely about being stubborn; it’s usually rooted in legitimate concerns. The absolute first step is to just listen. Sit down with them, ask open-ended questions, and understand their perspective without getting defensive.
Once you understand the "why" behind their hesitation, find the most respected clinical leaders within that skeptical group. Don't fight them—empower them. Make them your 'change champions' and let them lead small-scale pilots. When they see the benefits firsthand, their endorsement will be far more powerful than any top-down mandate. Exploring our real-world use cases can provide concrete examples to share with them.
Finally, you have to back them up with incredible support. This means personalized, hands-on training and having experts available to help when they get stuck. It's all about building confidence. When people feel capable, resistance naturally turns into adoption.
What is the best change management model for healthcare?
There isn't a single "best" model, but the most effective strategies today combine elements from several proven frameworks. Kotter's 8-Step Process is excellent for creating urgency and building a guiding coalition. The ADKAR Model (Awareness, Desire, Knowledge, Ability, Reinforcement) is invaluable for focusing on the individual's journey through change. The key is to be agile—use these models as a flexible toolkit, not a rigid script, adapting them to your specific organizational culture and the complexity of the change.
How can AI tools support change management in healthcare?
AI is a powerful enabler for a modern change strategy. For instance, AI tools for business can analyze workflows to pinpoint the biggest bottlenecks that a new system should solve, making the business case for change undeniable. During implementation, AI can personalize training materials for different roles and provide predictive analytics to identify staff who might be struggling with adoption. After launch, AI-powered dashboards can track KPIs in real-time, giving leaders the insights needed to adapt their strategy on the fly. This turns change management from a reactive process into a proactive, data-driven discipline.
Ready to build a resilient, future-ready healthcare organization? Ekipa AI provides the strategic framework and expert support to turn your vision into reality. Start building your tailored AI roadmap with our AI Strategy consulting tool or connect with our expert team to learn more.