A Guide to Modern Healthtech Software Transformation
Discover how healthtech software is revolutionizing patient care and operations. Our guide covers key categories, ROI, compliance, and AI-driven strategies.
Healthtech software is simply any technology—from an app on your phone to a complex hospital platform—designed to improve how healthcare is delivered, managed, and accessed. It’s the engine driving the shift from clunky, paper-based systems to a connected, data-driven world where patient care is more efficient, accessible, and personalized. This spans everything from digital patient records to AI tools that help doctors make better decisions.
The Digital Transformation of Healthcare
Imagine walking into a specialist’s office, and they already have your complete medical history, instantly. Or picture a world where smart algorithms help doctors catch diseases months or even years earlier, and you can see your doctor from your living room. This isn't science fiction; it's the reality that healthtech software is building right now. It's not just an IT upgrade—it’s a fundamental reimagining of the entire patient journey.
At its core, healthtech software tackles some of the industry’s most persistent headaches: crippling operational costs, rampant clinician burnout, and patient data that's scattered across a dozen different, disconnected systems. The market for these solutions is exploding, projected to reach over $100 billion by 2035, because the demand for efficiency and modern, digital experiences has never been higher. For any healthcare organization, this trend is impossible to ignore.
Why Healthtech Is Gaining Momentum
So, what's behind this massive push? A few key factors are at play. Today’s patients expect the same digital convenience from their doctor that they get from their bank. At the same time, providers are squeezed by the need to deliver better outcomes while keeping a lid on costs—something old-school manual processes just can't handle.
This pressure cooker environment has become a powerful catalyst for innovation. Healthtech gives providers smarter tools, cuts down on mind-numbing administrative work, and puts patients in the driver's seat of their own health. It’s a win-win that leads to both better medicine and a healthier bottom line. For more on this, check out our insights on Healthcare AI Services.
Healthtech is not merely about digitizing old processes. It’s about creating new, more intelligent workflows that enhance decision-making, automate routine tasks, and ultimately free up clinicians to focus on what matters most—the patient.
The Strategic Imperative for Businesses
For any modern healthcare organization, adopting this technology is no longer a "nice-to-have." It’s a strategic necessity for staying relevant and competitive. The right software can dramatically improve how you operate, boost patient satisfaction, and elevate the quality of care. The impact is clear when you look at how things like AI-powered healthcare communications are already changing the game.
The first step is figuring out what you want to achieve. By homing in on your biggest pain points and setting clear goals, you can build a roadmap for real change. Whether the goal is to improve diagnostic accuracy, make patient onboarding smoother, or launch a remote care program, the right software is the foundation for a more resilient and effective future.
Exploring the Core Categories of Healthtech Software
To really get a handle on the healthtech world, you have to know what it's built on. Healthtech software isn't one single thing; it’s more like a collection of specialized tools. Imagine a modern workshop where every tool has a specific job, but they all work together to create something better.
These software categories are the engines that make healthcare more efficient, improve patient outcomes, and link up the entire care experience. From managing patient data to holding virtual appointments, each piece is vital. Knowing what they do helps an organization figure out exactly where technology can make the biggest difference and invest smarter in the right healthcare software solutions.
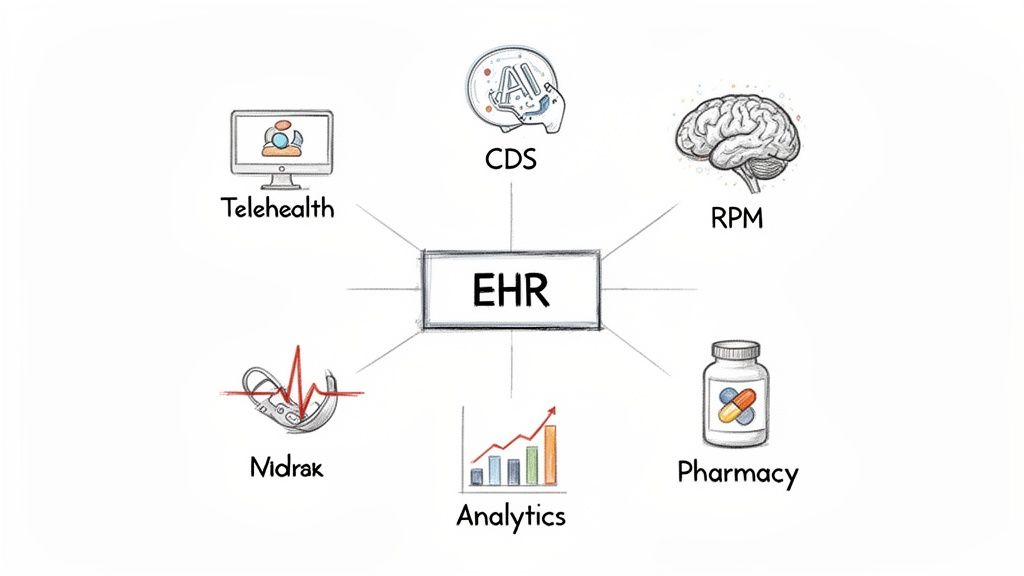
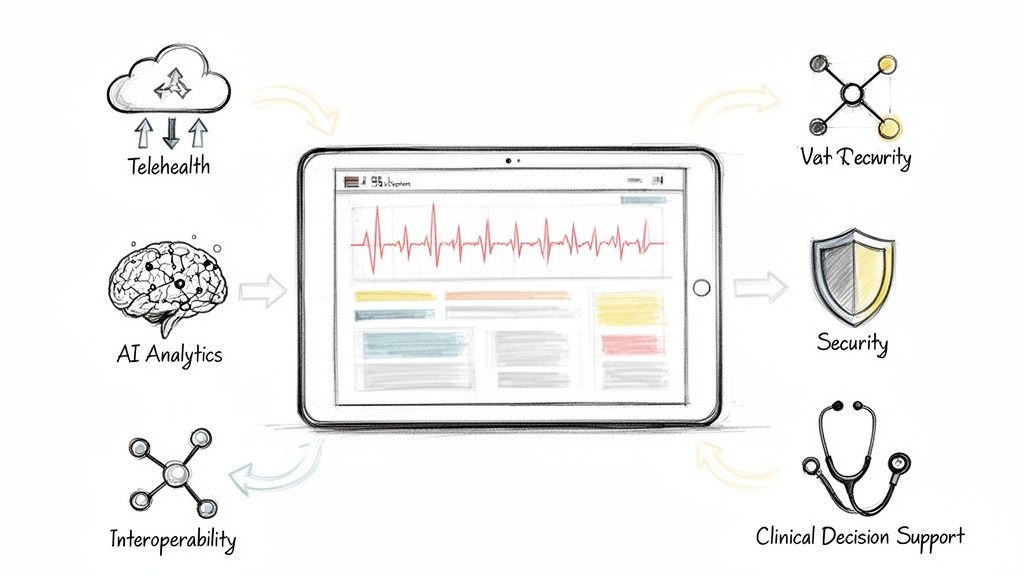
Electronic Health Records (EHR): The Digital Heartbeat
At the absolute center of almost any healthcare operation, you'll find Electronic Health Records (EHRs) and Electronic Medical Records (EMRs). These platforms are the digital version of a patient's entire medical chart, acting as the central nervous system for all their information. They pull everything—diagnoses, medications, lab results, immunization dates—into one secure, organized file.
The whole point is to create a single source of truth. This gives doctors, nurses, and specialists a complete and immediate picture of a patient's health, cutting down on medical errors, preventing redundant tests, and paving the way for better clinical decisions right on the spot.
Telehealth Platforms: Extending Care Beyond Clinic Walls
Telehealth software has gone from a fringe convenience to a core part of how care is delivered. These platforms use technology to make virtual visits, remote consultations, and ongoing patient communication happen. In many ways, they've become the new front door to the clinic, tearing down geographic barriers and making healthcare accessible to more people.
The upside goes well beyond just convenience. For patients managing chronic conditions or who have trouble traveling, telehealth offers a steady, reliable connection to their care teams. For providers, it helps optimize schedules, slash no-show rates, and serve a much wider group of patients without adding overhead.
By connecting patients and providers virtually, telehealth software doesn't just replicate an in-person visit—it creates a new, more flexible and continuous model of care delivery that fits modern lifestyles.
Clinical Decision Support (CDS): The AI Co-Pilot
Think of Clinical Decision Support (CDS) systems as an intelligent co-pilot for clinicians, often built directly into the EHR they’re already using. These tools analyze huge amounts of data in real-time to offer up helpful prompts, alerts, and evidence-based suggestions right when a decision is being made.
For instance, a CDS can flag a potential drug interaction before a prescription is written, suggest the right diagnostic tests based on a patient's symptoms, or alert a doctor if a care plan deviates from established best practices. This extra layer of intelligence helps reduce diagnostic mistakes, improve patient safety, and ensure everyone gets the best care possible. Seeing different real-world use cases can really bring to life how these tools are already making a difference.
Remote Patient Monitoring (RPM): Proactive and Continuous Insight
Remote Patient Monitoring (RPM) platforms bring healthcare right into the patient's home. Using connected devices—think smart blood pressure cuffs, glucose meters, or wearable sensors—RPM systems gather vital health data and send it securely back to the clinical team. This technology is what allows care to shift from being reactive to proactive.
Instead of waiting for a patient’s condition to get worse, clinicians can watch trends and step in at the first sign of trouble. This is a game-changer for managing chronic diseases like diabetes and hypertension, where that constant oversight can drastically reduce hospital readmissions and lead to better long-term health. Getting RPM right requires a clear plan, often developed through expert AI strategy consulting.
Analytics and AI Platforms: Uncovering Hidden Patterns
The most advanced frontier in healthtech software is all about analytics and Artificial Intelligence. These sophisticated platforms can digest enormous datasets from EHRs, medical images, and even public health statistics to find patterns and insights that would be completely invisible to the human eye.
This is the technology behind predictive models that can identify at-risk patients long before they show symptoms, and the algorithms that help hospitals run more efficiently. For any organization that wants to be a leader, finding the right AI tools for business and working with specialized Healthcare AI Services is how you turn all that raw data into a real competitive advantage. This is a major undertaking, but with guidance from our expert team, organizations can navigate the complexities and unlock incredible value.
For a quick overview, this table breaks down the main software categories and the value they bring to the table.
Key Healthtech Software Categories and Their Business Impact
| Software Category | Primary Function | Strategic Business Impact |
|---|---|---|
| EHR/EMR | Centralizes all patient health data into a single digital record. | Creates a unified source of truth, reducing medical errors and improving clinical efficiency. |
| Telehealth | Enables virtual consultations and remote care delivery. | Expands patient access, improves convenience, and optimizes provider schedules. |
| Clinical Decision Support (CDS) | Provides real-time, evidence-based alerts and recommendations to clinicians. | Enhances patient safety, improves diagnostic accuracy, and ensures adherence to best practices. |
| Remote Patient Monitoring (RPM) | Collects and transmits patient health data from their homes using connected devices. | Allows for proactive chronic disease management, reducing hospital readmissions and improving outcomes. |
| Analytics & AI | Analyzes large datasets to uncover insights, predict outcomes, and optimize operations. | Drives data-informed decision-making, identifies at-risk populations, and creates a competitive edge. |
Each of these categories represents a powerful tool on its own. When integrated, they create a healthcare ecosystem that is more connected, intelligent, and patient-focused.
How Healthtech Delivers Real Business Value and ROI
Let's be clear: investing in healthtech software isn't just about getting the latest and greatest tech. It’s a hard-nosed business decision aimed at generating a measurable return. The real value isn't found in a long list of features, but in the concrete results they deliver—from slashing operational costs to opening up new revenue streams.
For most organizations, the first and most obvious win is operational efficiency. Think about how much time is lost to administrative work. Scheduling, billing, and endless documentation can eat up as much as one-third of all healthcare costs. When you automate these repetitive tasks with smart internal tooling, you don't just cut overhead; you give your clinical staff their time back. They can focus on patients, not paperwork. This simple shift boosts productivity, improves job satisfaction, and reduces the high cost of staff burnout and turnover.
Boosting Revenue and Expanding Your Reach
But healthtech is more than just a cost-cutting tool. It's a powerful engine for growth. AI-powered diagnostic tools, for instance, can read medical images with a speed and accuracy that’s difficult for the human eye to match. This does more than improve patient outcomes—it dramatically increases throughput, allowing a clinic or hospital to see more patients and directly increase its revenue.
Telehealth platforms are another perfect example. They completely erase geographic barriers. Suddenly, you can serve patients in the next town over or even across the country, all without the massive capital investment of building a new physical clinic. Expanding your market like this is a straight line to more revenue and a stronger competitive edge.
Remote Patient Monitoring (RPM) also makes a very clear financial case. By keeping a close watch on patients with chronic conditions from their own homes, providers can step in at the first sign of trouble. This proactive approach helps prevent expensive emergency room visits and hospital stays.
A single prevented hospital readmission can save thousands of dollars. The ROI on RPM technology is not just clear, it's often immediate. You're turning a major cost center into a source of savings while improving long-term patient health.
The Economic Case for AI in Healthtech
The financial impact of modern healthtech, especially when powered by artificial intelligence, is impossible to ignore. AI is supercharging revenue efficiency. Healthtech startups are now hitting $100M-$200M ARR in under five years—a milestone that used to take traditional software companies a decade or more. They're also posting incredible gross margins of 70-80% by treating AI as 'services-as-software'. (Source)
This incredible speed-to-value shows just how important it is to have a solid game plan. Without expert guidance, it's easy to end up with a collection of disconnected tools that never deliver on their promise. That's where strategic AI strategy consulting comes in. It's about connecting every technology investment to a specific business goal, making sure every dollar you spend moves the needle. A well-thought-out plan, like a Custom AI Strategy report, identifies the highest-impact opportunities and puts them first.
For organizations ready to move past manual work, AI Automation as a Service provides a direct path to these efficiencies without needing a massive in-house development team. In the end, you get real business value from healthtech when you treat it not as just another tool, but as a central part of your business strategy. This approach is key. With the right plan and the right partners, the ROI isn't just a number on a spreadsheet—it becomes a powerful driver of both your financial health and clinical excellence.
Navigating Healthtech Regulation and Cybersecurity
Innovation in healthtech is exciting, but it comes with a heavy dose of responsibility. The moment you move patient data into the digital world, you’re not just dealing with code and features; you're handling people's most private information. For any leader in this space, getting the rules right isn’t just a box-ticking exercise—it’s the bedrock of patient trust and legal survival.
This isn’t like building a social media app. You can’t just launch and patch later. Every database, every API, and every user interface has to be designed with compliance baked in from the very first sketch. Think of it as building a bank vault; you don’t build the walls and then wonder how to add a lock. The security and regulatory requirements must be part of the initial blueprint.
The Pillars of Healthtech Compliance
When it comes to protecting patient data, a couple of major regulatory frameworks dominate the conversation. Even if you only operate in one region, it’s smart to understand both, as their principles are shaping global standards.
- HIPAA (Health Insurance Portability and Accountability Act): In the United States, HIPAA is the law of the land for patient privacy. It sets the rules for how protected health information (PHI) can be used, stored, and shared. If you have users in the U.S., HIPAA isn’t optional—it’s mandatory.
- GDPR (General Data Protection Regulation): Don't let its European Union origins fool you; GDPR has long arms. If your service processes the personal data of anyone in the EU, you have to follow its strict rules on data privacy, user consent, and individual rights.
These regulations are more than just legal red tape. They are a guide to building technology that people can actually trust. Proving you're compliant isn't just a defense—it's a competitive advantage that shows you take patient safety seriously.
Cybersecurity: Your Unbreakable Shield
Compliance is about playing by the rules. Cybersecurity is about actively defending your goal. The healthcare industry is a massive target for cybercriminals, and the cost of a breach is staggering. We're talking an average of $11 million per incident, which is higher than any other sector. A single attack can result in crippling fines, lawsuits, and a loss of patient trust that you may never recover.
Protecting this sensitive data demands a multi-layered defense built directly into your healthtech software. This goes way beyond asking users for a strong password. You need end-to-end encryption for data in transit and at rest, rock-solid access controls to ensure only authorized personnel see what they need to, and constant vulnerability scanning to patch holes before attackers find them. When moving to the cloud, for instance, a deep understanding of Security-First Cloud Compliance: Best Practices for HIPAA becomes absolutely essential.
Building secure software is a marathon, not a sprint. It’s a continuous commitment that starts on day one and never really ends. This security-first mindset has to be woven into every stage of development, from the initial brainstorming sessions to long-term maintenance. Trying to bolt security on after the fact is like trying to install a fire sprinkler system after the house is already built—it’s messy, expensive, and never as effective.
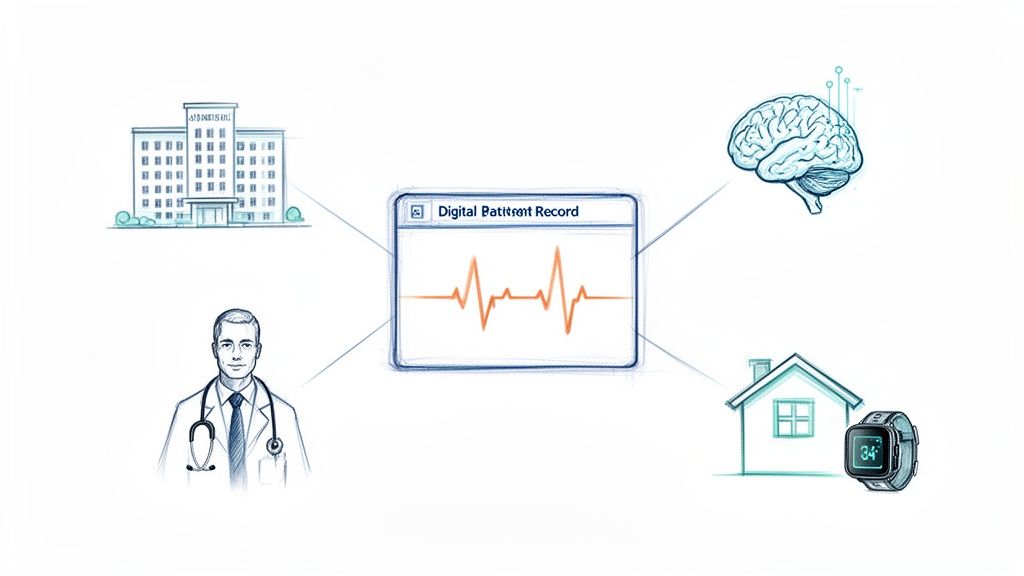
Making Sure Your Systems Talk to Each Other: The Interoperability Challenge
A brand-new, powerful piece of healthtech software is essentially useless if it just becomes another island of data. Picture a hospital where the ER, the lab, and the pharmacy all run on different systems that can’t communicate. What you get is a chaotic, inefficient mess. Critical information gets lost, leading to repeated tests, delayed care, and burned-out clinicians. This is the core problem that interoperability solves.
Think of interoperability as the universal translator for healthcare data. It’s the behind-the-scenes work that lets completely different software—from a hospital’s massive EHR system to a patient's simple fitness tracker—speak the same language. Without it, you have a pile of expensive, disconnected tools. With it, you get a single, cohesive stream of information that paints a complete picture of a patient's health.
Building this connected ecosystem is the end goal, and it’s being pushed forward by both new technology and government regulations. The money is following, too. The global healthcare software market is on track to hit $38.5 billion by 2026 and is projected to soar past $100 billion by 2035, growing at an explosive 10.34% CAGR. This boom is largely thanks to AI, cloud computing, and a shared understanding that all these systems simply must work together. You can explore more healthcare software market trends here.
The Building Blocks: APIs and FHIR Standards
So, how do we actually build this universal translator? The two key pieces of the puzzle are Application Programming Interfaces (APIs) and industry-wide standards, especially FHIR (Fast Healthcare Interoperability Resources).
- APIs are like secure messengers. They let different software applications ask for and share specific bits of information without needing to know the complex inner workings of the other system.
- FHIR provides the common language and rules for that conversation. It defines a standard way to structure health data, so when one system sends a "patient allergy," the receiving system knows exactly what that means.
Together, APIs and FHIR lay the groundwork for a truly connected health network. They give developers the tools to build new apps that can securely "plug into" existing EHRs and other platforms, pulling and pushing data to create more complete, useful experiences for both patients and doctors. Any serious AI Product Development Workflow has to be built with this kind of integration in mind from day one.
True interoperability means a doctor can see a patient’s entire story—from their family physician to a specialist visit to the pharmacy—all in one unified view. This 360-degree perspective gets rid of the guesswork and gives providers the confidence to make faster, safer, and better-informed decisions.
Why a Connected System is a Strategic Win
Getting your systems to talk to each other delivers some serious strategic advantages. When data moves freely and securely, clinicians finally get the full context they need to make the right call, which cuts down on diagnostic mistakes and avoids redundant, expensive procedures. It also puts power back in the hands of patients, allowing them to securely access and share their own health records through patient portals and mobile apps.
Beyond that, a connected data environment is the jet fuel for advanced analytics and AI. You can't possibly predict patient outcomes or find operational efficiencies if your data is locked away in a dozen different formats across disconnected systems. Interoperability breaks down those walls, making it possible to find the kinds of deep insights that drive real innovation. For example, an AI-powered data extraction engine can pull structured information from countless sources to feed predictive models, but that’s only possible if it can get to the data in the first place.
Your Roadmap to a Successful Healthtech Implementation
Taking on a healthtech transformation is a serious commitment. But with a clear roadmap, what seems like a massive project becomes a series of achievable steps. A successful rollout isn't just about plugging in new software; it's a strategic shift that redefines how your teams work and requires buy-in from the top down. The real work begins long before you ever see a product demo.
The very first step is to get crystal clear on your core business objectives. What specific problem are you actually trying to solve? Are you aiming to slash administrative overhead by 20%? Or maybe you need to speed up diagnostic turnaround times or cut down on patient no-shows. When you start with a clear, measurable goal, every decision that follows will be laser-focused on delivering a tangible outcome, as we explored in our AI adoption guide.
Assembling Your Cross-Functional Team
A healthtech project will fail if it's siloed. You absolutely need a dedicated, cross-functional team with people from every key department. This group should include the clinical staff who will be using the software every single day, the IT experts who know your current infrastructure inside and out, and the administrative leaders who can champion the project and manage the budget.
Bringing your end-users into the conversation from the very beginning is non-negotiable. Their early involvement is one of the best predictors of whether the new system will be adopted or rejected. This team will be your boots on the ground, helping evaluate solutions and ensuring the tech you choose solves real-world problems for the people who need it most.
A key technical consideration for this team will be interoperability—making sure new software can talk to your existing systems. The flow below shows how modern standards like FHIR create that seamless connection.
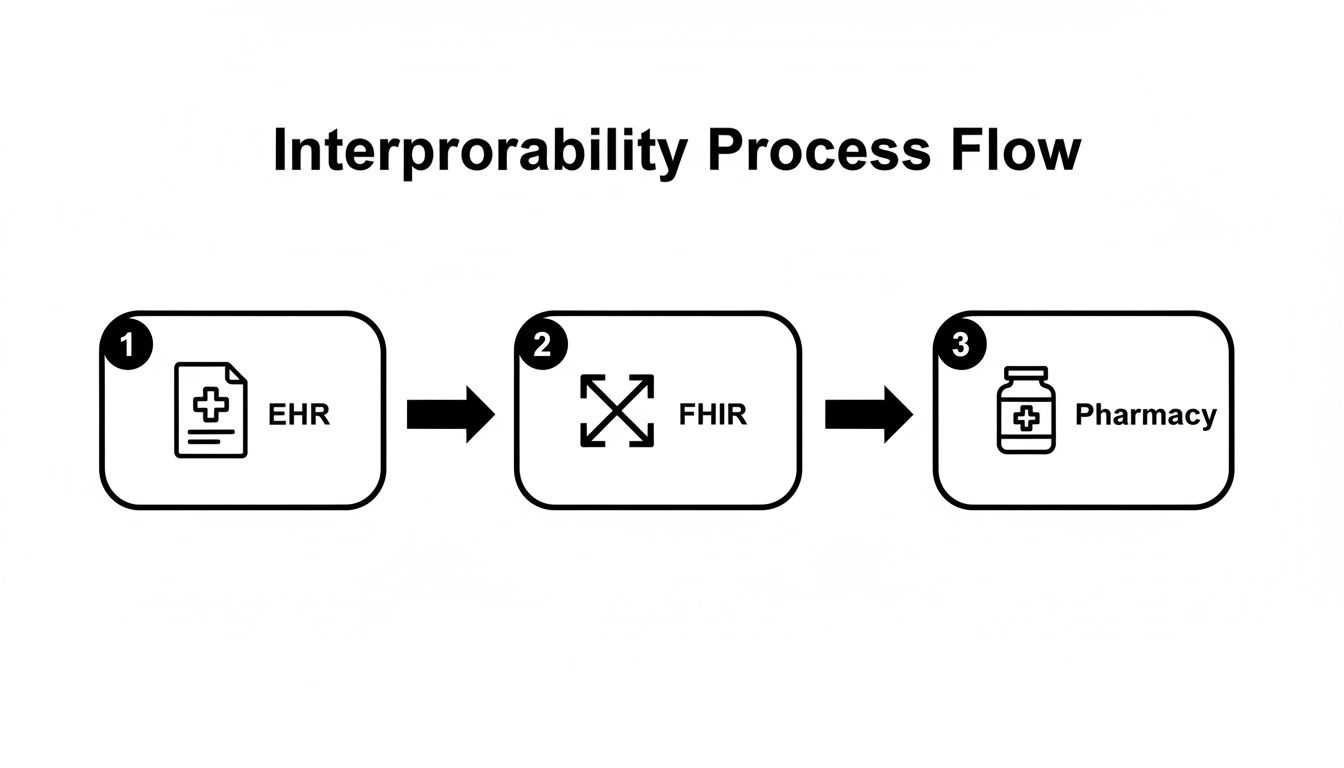
This illustrates how critical patient information can move securely from an EHR to a pharmacy, ensuring care is never fragmented.
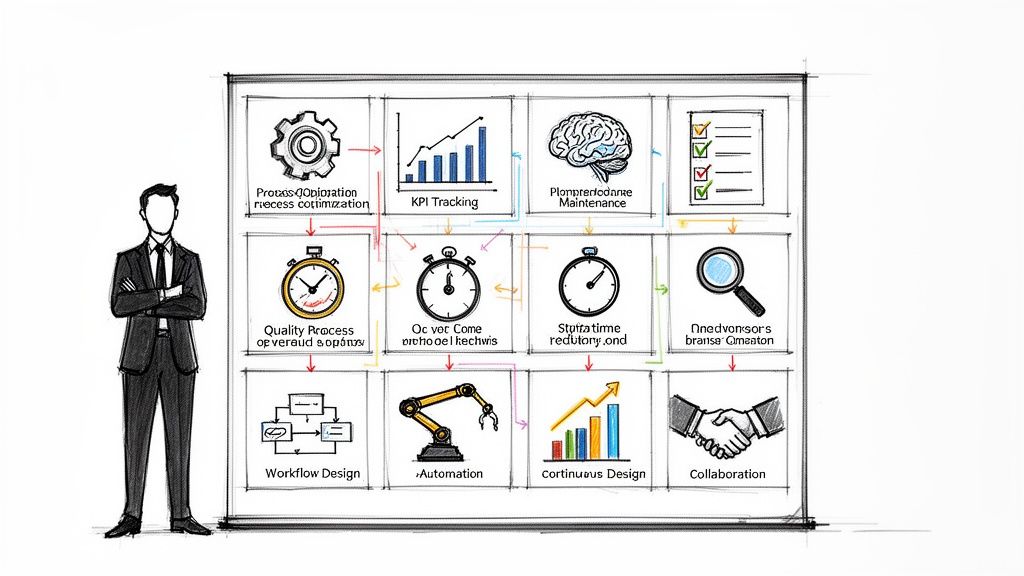
The Implementation Journey Step-by-Step
Once you have your goals defined and your team assembled, the path forward starts to look much clearer. A structured approach ensures nothing important falls through the cracks.
- Vendor Selection and Due Diligence: Don't just look at the shiny features. Evaluate potential partners against a strict checklist. Scrutinize their solution’s security protocols, integration capabilities, and scalability. Most importantly, look beyond the initial price tag to understand the total cost of ownership. You want a partner who gets healthcare, not just tech.
- Pilot Program and Testing: Before you flip the switch for everyone, launch a limited pilot program with a small, controlled group of users. This is your chance to find workflow hiccups, gather honest feedback, and squash bugs before they affect the entire organization. A well-planned pilot is your best defense against a chaotic launch.
- Training and Change Management: The technology itself is only half the equation. You have to invest heavily in comprehensive, role-specific training. Even more critical is a solid change management plan that communicates the "why" behind the new system, addresses people's fears, and shows them how this change will ultimately make their jobs easier.
- Go-Live and Post-Implementation Support: The launch day isn't the finish line; it's the starting line. Make sure your vendor provides robust, ongoing support after you go live. You'll need to continuously monitor system performance, gather user feedback, and make iterative improvements. A great implementation is a process of constant optimization.
The market for this technology is exploding. The intelligent medical software market is expected to jump from $4.79 billion in 2025 to a staggering $22.33 billion by 2035, growing at a 16.64% CAGR. This incredible growth shows just how critical a well-managed implementation is to stay competitive.
Navigating this entire process can feel overwhelming, but you don't have to do it alone. Getting expert guidance can provide the clarity and resources you need to move faster and with more confidence. For a deeper dive into managing a complex tech rollout, you might find our insights on the AI implementation workflow helpful. By following a structured roadmap, you can steer your organization through the journey and achieve a truly successful transformation.
FAQs on Healthtech Software Adoption
If you're an enterprise leader exploring healthtech, you've probably got a lot of questions. Let's tackle some of the most common ones with straightforward, practical answers to help you map out your next move.
Where Do We Even Begin?
The most critical first step has nothing to do with technology. It's about getting crystal clear on your business goals. Before you demo a single platform, you need to pinpoint the specific, measurable problems you're trying to solve.
Are you aiming to slash administrative costs by 20%? Or maybe you need to accelerate diagnostic turnaround times. A well-defined objective is your North Star for the entire project.
This is where an initial AI strategy consulting phase can be a game-changer. It helps connect your organization's unique pain points to the right solutions, involves a deep AI requirements analysis, and builds a solid foundation to ensure every dollar you spend is tied to a real-world outcome.
How Do We Get Our Team to Actually Use It?
User adoption is the make-or-break factor for any new healthtech tool. The secret isn't a great rollout plan—it's involving your clinicians and administrative staff from day one.
Bring them into the selection process. Let them tell you what works and what doesn't in their daily routines. Prioritize software with an intuitive, clean interface and don't skimp on role-specific training. A solid change management plan that shows your team exactly how this new system makes their lives easier is just as vital as the tech itself.
Should We Build Our Own Solution or Buy an Off-the-Shelf Product?
Ah, the classic "build vs. buy" debate. There's no single right answer, but here's how to think about it. Off-the-shelf software gets you up and running faster with lower upfront costs, making it a great option for solving common industry problems.
On the other hand, custom healthcare software development delivers a solution built just for you. It can become a powerful competitive advantage by perfectly matching your specific workflows and care models. While it's a bigger investment of time and money, a custom solution can deliver far greater value in the long run.
Often, the sweet spot is a hybrid approach: start with a commercial platform and then build custom modules on top of it. This gives you the best of both worlds—speed and a perfect fit.
What is the difference between HIPAA and GDPR?
Think of it this way: HIPAA is a specialist, focused only on protecting health information in the U.S. GDPR is a generalist with a global reach, covering all types of personal data for EU residents and giving them specific rights over how it’s used.
How can we ensure our software remains compliant over time?
Compliance isn't a one-and-done project. It requires constant vigilance. This means performing regular risk assessments, continuously monitoring your systems for threats, and keeping a close eye on any changes to the regulations. Just as important is training your team—everyone who touches patient data needs to know the rules and their role in protecting it.
What are the biggest cybersecurity threats in healthtech?
The classic threats are still the most dangerous: phishing emails tricking employees into giving up their credentials, ransomware that encrypts critical patient files and holds them hostage, and data breaches caused by insecure code. A strong defense always combines technical tools with human education. Your people are your first and last line of defense.
Ready to build a clear, actionable AI strategy for your healthcare organization? Ekipa AI delivers a Custom AI Strategy report in just 24 hours, turning your business goals into a concrete implementation roadmap. For a more personal touch, get to know our expert team who can guide you every step of the way.