Accelerating Outcomes with Healthcare Decision Enablement in AI-Driven Care
Explore how healthcare decision enablement using AI boosts patient care and efficiency. Learn practical steps for successful implementation.
Picture a GPS for healthcare. But this isn't just any GPS—it's one that sees traffic jams before they happen, suggests smarter routes on the fly, and flags potential hazards long before you get there. This is the essence of healthcare decision enablement, a fundamental shift away from reactive treatment and toward a proactive, predictive model of care. It’s all about getting the right information to the right person at exactly the right moment.
What Is Healthcare Decision Enablement?
Simply put, healthcare decision enablement is the practice of arming clinicians, administrators, and even patients with timely, relevant, and actionable insights so they can make better choices. We're not talking about dumping raw data on their laps. The goal is to deliver synthesized intelligence directly into their daily workflows to boost clinical outcomes, streamline operations, and enhance patient safety.
This approach tackles some of the most stubborn problems in healthcare head-on. Think about it: diagnostic delays, frustrating operational bottlenecks, and wasted resources often happen because people are either drowning in data or don't have the clear, data-driven guidance they need. Decision enablement cuts through that noise, acting like a filter that highlights what truly matters.
Moving Beyond Traditional Support Systems
For decades, the industry has leaned on Clinical Decision Support (CDS) systems. You've probably seen them inside electronic health records (EHRs), popping up with rule-based alerts and reminders. They can be helpful, but their limitations are clear. These systems often lead to "alert fatigue," where busy clinicians start tuning out the constant, low-value notifications.
Healthcare decision enablement is the next logical step. It weaves in advanced analytics and intelligent AI solutions to offer a much deeper, more contextual level of insight. So, instead of just flagging a possible drug interaction, a true enablement system might predict a patient’s risk of developing sepsis in the next 12 hours based on subtle, almost imperceptible changes in their vitals.
This marks a huge change in mindset. It's about moving from simply presenting data to actively guiding decisions. Information stops being a passive resource and becomes an active partner in the care process, sharpening the judgment of skilled professionals.
The Strategic Importance for Modern Healthcare
With costs soaring and patient cases getting more complex, making the best possible decision every time isn't just a goal—it's an absolute necessity. Every single choice, whether it's a treatment plan for one patient or a staffing schedule for the entire hospital, sends ripples across quality, cost, and patient experience.
When done right, decision enablement creates a cascade of benefits:
For Clinicians: It lightens the mental load. The system surfaces the most critical patient data, suggests potential diagnoses, and points toward evidence-based treatment plans.
For Administrators: It provides a crystal ball for things like patient flow, resource needs, and supply chain demands, allowing them to manage proactively instead of constantly fighting fires.
For Patients: It empowers them with personalized information about their own health and treatment options, turning them into active participants in their care.
At its heart, healthcare decision enablement helps to improve critical thinking skills by giving professionals the tools to make sense of complex information and act decisively. Pulling this off requires a clear, cohesive plan, which is where expert AI strategy consulting often comes in to ensure the technology aligns perfectly with clinical and operational goals. By turning data from a burden into a strategic asset, organizations can build a healthcare system that's more resilient, efficient, and truly centered on the patient.
The Three Pillars of a Decision Enablement Framework
A truly effective healthcare decision enablement strategy rests on three core pillars. Think of it like a three-legged stool—if one leg is wobbly, the whole thing comes crashing down. These pillars are pristine data, intelligent analytics, and seamless workflow integration.
Getting this framework right is the first real step toward building a system that actually delivers. We need reliable, timely, and actionable insights for everyone, from the executive team steering the ship to the clinician on the front lines. Without a solid foundation across all three areas, even the most expensive technology will just be spinning its wheels.
Pillar One: Foundational Data Quality
Data is the fuel for this entire engine. But just having mountains of it isn't the point; the quality, accessibility, and governance of that data are absolutely non-negotiable. It's like trying to cook a five-star meal—you simply can't create a masterpiece with subpar ingredients, no matter how brilliant the chef is.
In a hospital or clinic setting, this means making sure that data from Electronic Health Records (EHRs), lab results, imaging scans, and even patient-reported feedback is clean, standardized, and easy to access. This is a huge undertaking, often requiring serious investment in infrastructure like custom healthcare software development just to break down the silos and create a single source of truth. The market for healthcare data technology reflects this push, valued at USD 3.10 billion in 2024 and projected to hit USD 9.5 billion by 2033. It's clear the industry is scrambling to unify these fragmented datasets, as detailed in market research from Grandview Research.
This image really drives home the challenges that a strong data foundation is meant to solve.
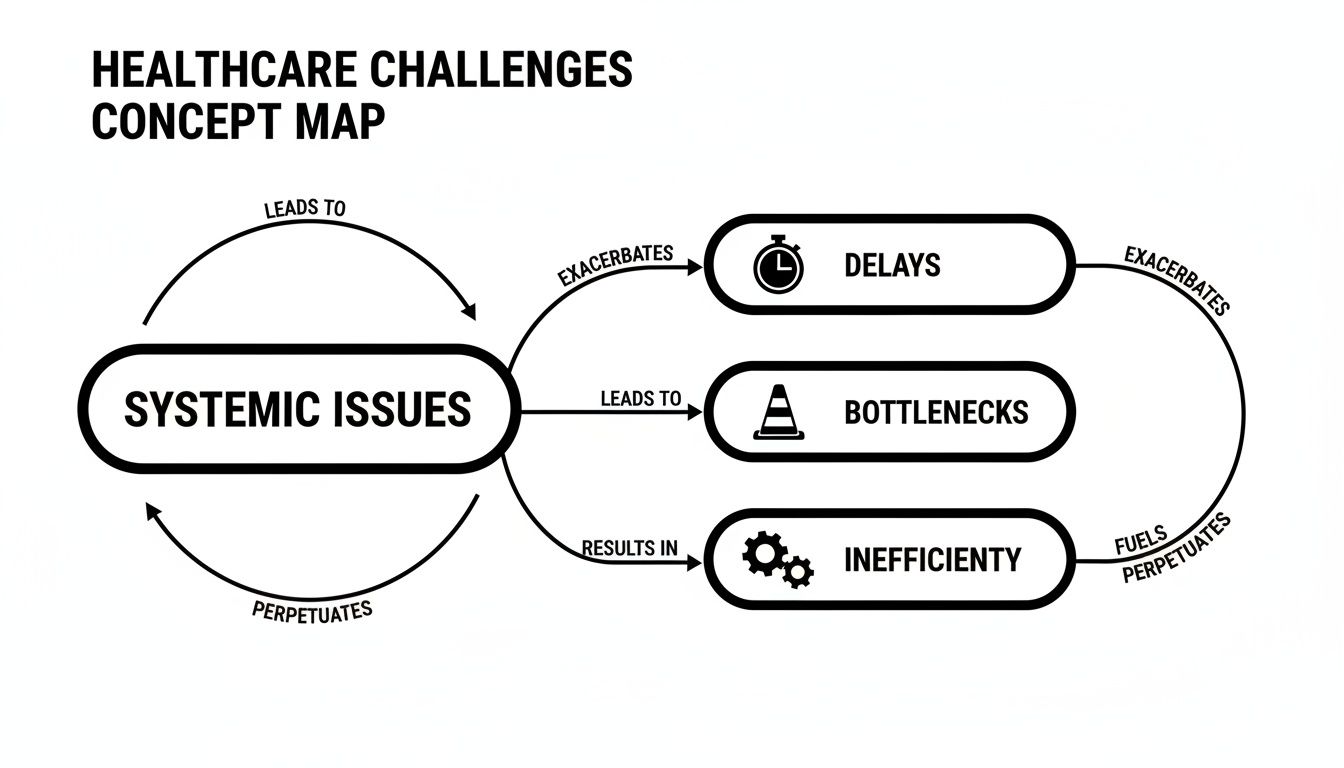
You can see how delays, bottlenecks, and general inefficiency are often a direct result of messy data management. It creates a vicious cycle that’s nearly impossible to escape without a complete overhaul.
Pillar Two: Intelligent Analytics
Once you have a reliable stream of high-quality data, the next step is to make it smart. This is where raw information gets transformed into forward-looking insights. The goal is to move beyond basic descriptive analytics (telling you what already happened) and into the far more valuable realms of predictive (what’s likely to happen next) and prescriptive (what you should do about it) models.
This is where sophisticated AI solutions really come into play. A traditional dashboard might show you that patient readmission rates are up this quarter. That's interesting, but not very helpful. AI-powered analytics, on the other hand, can pinpoint which specific patients are at the highest risk of being readmitted in the next 30 days and even suggest personalized steps to prevent it.
This pillar is the "intelligence engine" of decision enablement. It's the part that sifts through millions of data points to find the subtle patterns and hidden correlations that a human could never spot alone.
Pillar Three: Seamless Workflow Integration
This final pillar is arguably the most critical. You can have the most brilliant, world-changing insight, but if it doesn't reach the right person at the right time in a way that makes sense to them, it's completely useless. An alert that forces a busy doctor to log out of their EHR and open a separate dashboard is an alert that's going to be ignored. Period.
True integration means embedding these data-driven recommendations directly into the tools people already use every day. A sepsis risk score shouldn't be buried in a report; it should pop up right in the patient's chart, along with clear, actionable steps for the care team. This is often accomplished by building thoughtful internal tooling that enhances—rather than interrupts—the daily grind of healthcare professionals.
Success comes down to making the smart choice the easy choice. By weaving insights directly into the fabric of daily operations, you ensure that data-driven guidance isn't just available, but is actively used to improve every single decision. It's this holistic approach, as we explored in our AI adoption guide, that unlocks real, lasting change.
How AI Transforms Healthcare Decision-Making
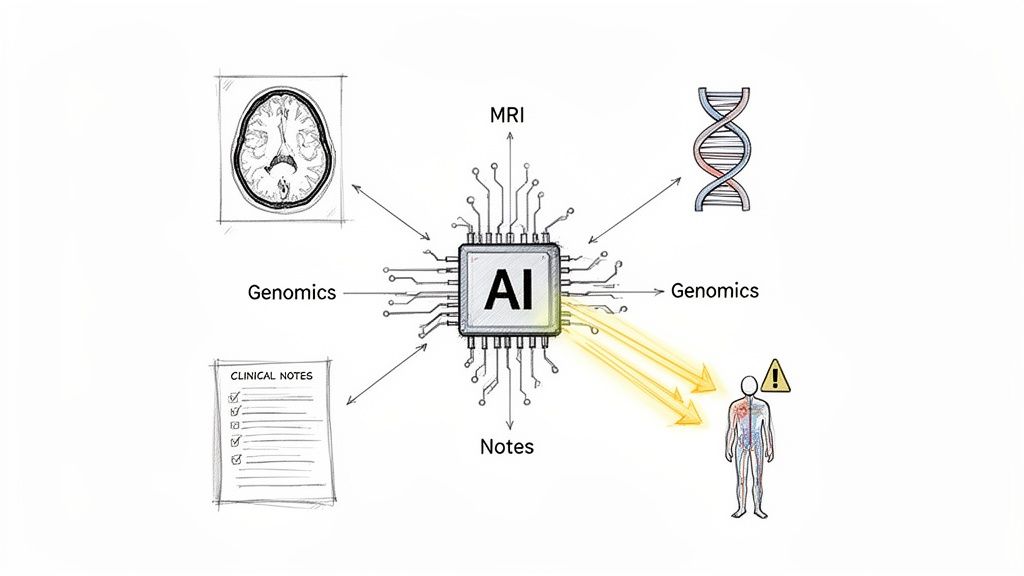
Think of artificial intelligence as the engine that finally brings healthcare decision enablement to life. It’s what moves the concept from a nice idea on a whiteboard to a practical tool in the hands of clinicians and administrators. AI algorithms have an almost superhuman ability to sift through massive, complex datasets—the kind that would completely swamp a human analyst. We're talking about finding the hidden, meaningful patterns buried within millions of MRI scans, genomic sequences, and messy, unstructured clinical notes.
This incredible capacity allows AI to act as both an advanced early warning system and a powerful diagnostic partner. Instead of just reacting to symptoms as they appear, healthcare systems can start to anticipate them, making care far more proactive and effective.
From Data Overload to Actionable Intelligence
At its core, AI's job here is to turn the overwhelming firehose of healthcare data into a clear, usable signal. A single physician can’t possibly keep up with every new medical study published or manually track every tiny fluctuation in a patient's vitals around the clock. AI can. It constantly learns from new information and flags only what truly matters, bringing the signal out of the noise.
This shift is changing the game. Organizations that don't get on board with the rapid adoption of AI are going to get left behind. In this environment, doing nothing is no longer a safe bet.
AI's true value isn't just about processing data faster; it's in revealing insights that were previously completely invisible. It connects the dots across different sources to build a richer, more complete picture of both patient health and operational efficiency.
The market is clearly responding. The global AI in healthcare market is valued at USD 36.96 billion as of 2025 and is on track to grow more than 16 times in the next decade. Physician adoption is surging, too, jumping from 38% in 2023 to 66% in 2024. That’s a massive 28-percentage-point increase in just one year, as highlighted in recent U.S. digital health statistics. You can explore more on these adoption trends at accretiveedge.com.
Concrete Examples of AI in Action
Let's ground this in reality. Here are a few real-world examples of how different types of AI are helping people make better decisions right now:
Predictive Models: Imagine a model analyzing real-time data from an ICU patient's monitors and electronic health record. By spotting subtle patterns that often precede a crisis, it can flag a patient at high risk for sepsis hours before a human might notice. This gives the clinical team a critical head start to intervene.
Computer Vision: In radiology, AI-powered computer vision can review thousands of medical images in minutes. These tools don't replace the radiologist; they act as a tireless assistant, prioritizing urgent cases by flagging scans with suspected abnormalities for immediate human review.
Natural Language Processing (NLP): An NLP model can read and make sense of unstructured text from doctors' notes, patient histories, and research papers. This unlocks critical information—like signals of adverse drug events or trends in patient sentiment—that would otherwise be buried in dense text files.
AI Impact on Key Healthcare Decisions
Bringing these AI capabilities into the daily workflow has a direct and measurable impact on decisions across the entire healthcare system. By introducing smart automation and predictive insights, organizations can fundamentally improve how they operate.
To give you a clearer picture, this table compares the old way of doing things with the new, AI-enabled approach.
AI Impact on Key Healthcare Decisions
| Decision Area | Traditional Approach (Without AI) | AI-Enabled Approach | Key Business Outcome |
|---|---|---|---|
| Patient Triage | Manual assessment based on presented symptoms and staff judgment. | AI analyzes symptoms, vitals, and history to predict severity and recommend care. | Reduced wait times and improved patient flow. |
| Treatment Planning | Relies on physician experience and generalized clinical guidelines. | AI analyzes patient genomics and history to suggest personalized treatment paths. | Higher treatment efficacy and better outcomes. |
| Hospital Staffing | Based on historical averages and reactive adjustments. | Predictive models forecast patient admissions to optimize staffing levels. | Lower labor costs and reduced staff burnout. |
| Claims Processing | Manual review of claims, leading to errors and delays. | AI automatically flags fraudulent or inaccurate claims for review. | Faster reimbursement and reduced admin waste. |
As these examples show, AI isn't some far-off, futuristic concept. It's a practical tool delivering real value today. Tools like the Clinic AI Assistant and other AI tools for business are specifically built to bring this level of intelligence to the front lines of patient care, making these advanced capabilities both concrete and achievable for organizations ready to take the next step.
Putting It Into Practice: Use Cases Across the Healthcare Value Chain
Theory is one thing, but to really understand the impact of healthcare decision enablement, you have to see it in action. When you move past the concepts and look at real-world applications, you start to see its tangible value across clinical work, hospital operations, and even patient interactions. These examples show how well-placed AI tools can solve specific, high-stakes problems, leading to real improvements in efficiency, costs, and the quality of care.
The pattern is usually pretty straightforward: a stubborn, recurring problem gets a smart, data-informed solution, and the result is a significant positive change. This simple framework is a great way for leaders to spot the best starting points for AI within their own organizations.
Clinical Applications Driving Precision and Speed
In a clinical setting, decision enablement has a direct line to patient outcomes. It’s all about giving providers a clearer, deeper view into the data. The goal isn’t to replace human expertise but to enhance it, helping clinicians catch critical details that might otherwise get lost in the daily information overload.
A fantastic example of this is precision medicine. We're moving away from one-size-fits-all treatments. Instead, AI models can analyze a patient’s unique genetic makeup, lifestyle, and medical history to recommend therapies with the highest chance of success for that specific person. This cuts down on the painful trial-and-error process and gets patients on effective treatments faster.
Another game-changer is clinical trial matching.
The Problem: One of the biggest hurdles in medical research is simply finding the right patients for a trial. Doing it manually is slow, inefficient, and often misses people who could benefit, which delays the arrival of new treatments.
The Solution: AI algorithms can sift through millions of electronic health records in moments, automatically flagging patients who fit the complex criteria for a given study.
The Impact: This massively speeds up recruitment, which lowers research costs. More importantly, it gives patients access to potentially life-saving experimental treatments they might never have known existed.
Operational Enhancements for a Smarter System
Beyond the exam room, decision enablement is overhauling hospital operations. It tackles the bottlenecks and inefficiencies that inflate costs and lead to staff burnout. At the end of the day, smooth operations are the foundation of good care, and AI gives us the tools to manage these complex systems proactively instead of reactively.
Take the classic challenge of emergency department (ED) patient flow. EDs are often chaotic, with unpredictable waves of patients causing long wait times and dangerous overcrowding. Using predictive analytics, a hospital can now forecast patient volume based on historical data, the time of day, and even what’s happening in the local community.
This allows administrators to get ahead of the curve, optimizing staffing and resources before a rush hits. It transforms the environment from constant fire-fighting to something much more controlled and efficient. The payoff? Shorter waits for patients and a less stressful shift for the staff.
Along the same lines, claims processing is an area begging for an upgrade. This administrative slog is famously manual, slow, and full of errors, which causes costly payment delays and denials. With AI-powered automation, systems can instantly review claims, flag potential mistakes or fraud, and approve clean claims on the spot. This slashes administrative waste and gets revenue flowing much faster.
Patient-Facing Initiatives for Engagement and Empowerment
Finally, decision enablement is reaching patients directly, helping them shift from being passive recipients of care to active partners in their own health. When people get personalized, timely information, they are far more likely to stick to their treatment plans and make healthier choices.
Smart platforms can now send personalized health reminders and educational content right to a patient’s phone. A person with diabetes, for example, might get a nudge to check their blood sugar, followed by a link to a heart-healthy recipe. This kind of ongoing, tailored support is invaluable for managing chronic conditions between appointments.
This approach forges a more connected and supportive care experience. We dig deeper into this in our overview of Healthcare AI Services, which explains how technology can foster much stronger patient-provider relationships. These tools don't just improve health outcomes; they build patient loyalty and trust.
A Strategic Roadmap for Implementation
Getting from an idea to a fully integrated decision enablement solution can feel overwhelming. The key is to break the journey down into manageable, logical phases. Think of it less like a sprint and more like a carefully planned expedition. This roadmap will walk you through the critical steps, from the initial "what if?" to a fully scaled, governed system that delivers real value.
Of course, any successful journey needs a capable guide. Strong leadership is non-negotiable, which is why sharpening business skills for healthcare leaders is so critical. With the right people and a solid plan, your organization can move forward with confidence.
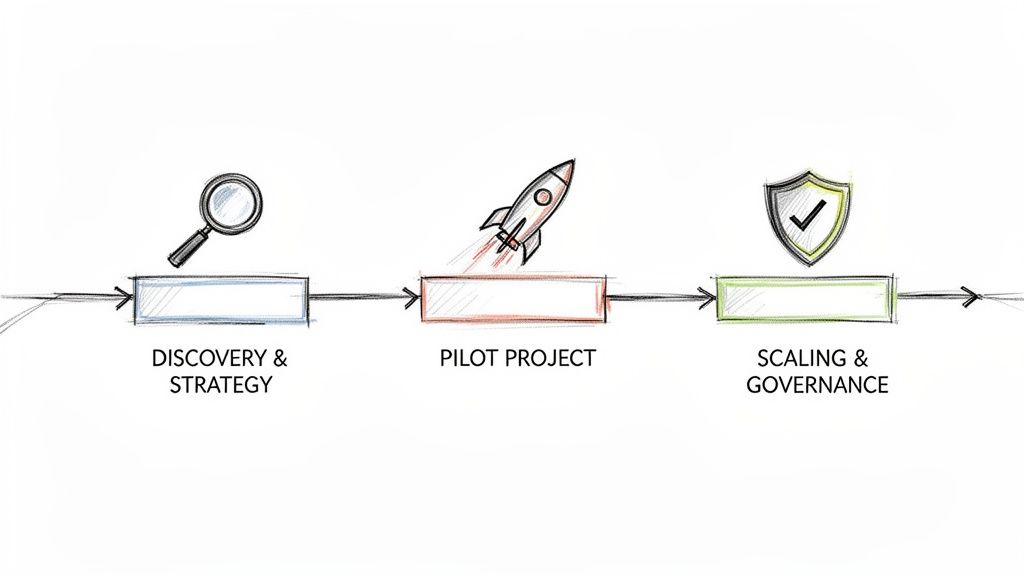
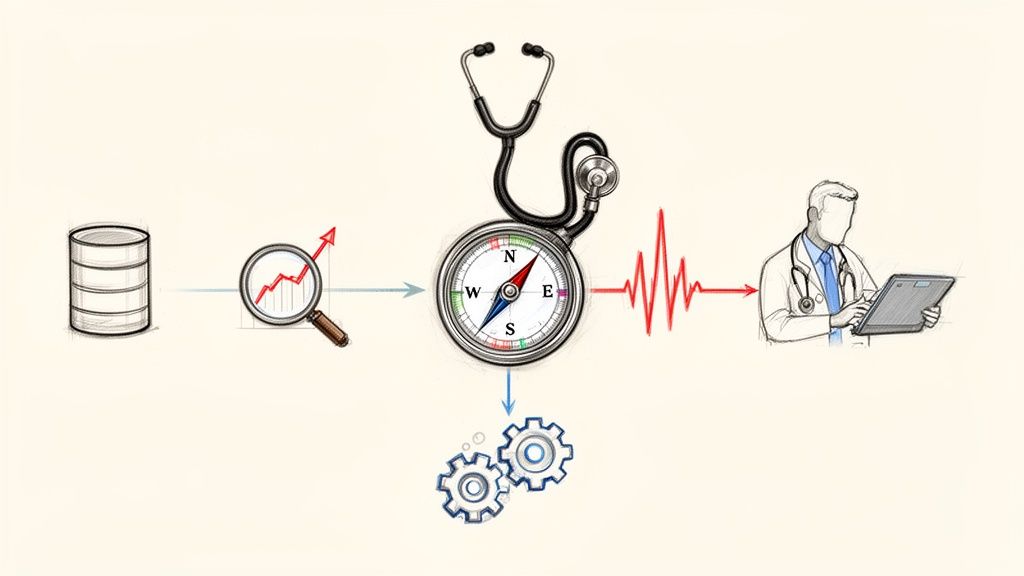
Stage One: Discovery and Strategy
Before you build anything, you need a blueprint. This first stage is all about a deep, honest look at your organization’s biggest pain points and clearest opportunities. What does success actually look like for you?
This isn't about vague goals. It's about defining concrete objectives that will act as your north star. Are you aiming to cut patient readmission rates by 15%? Or maybe your focus is on optimizing operating room schedules to boost utilization. Getting these specifics down on paper is the first, most important step. Without this clarity, projects tend to meander, burning through time and money with little to show for it. You can start building your strategy with a Custom AI Strategy report.
Stage Two: The Pilot Project
With a solid strategy defined, it's time to prove the concept. A pilot project is your chance to get a quick win, demonstrating tangible value to build momentum and get stakeholders excited. You want to pick a project that’s high-impact but relatively low-risk.
Think small and focused. For instance, a hospital could pilot an AI tool that predicts patient no-shows, but only for a single outpatient clinic to start. It’s a contained problem with a clear, measurable outcome. Sticking to a structured AI Product Development Workflow keeps the pilot on track from design to deployment. A successful pilot isn't just a technical achievement; it's the most powerful evidence you can present for why this technology is worth the investment.
Stage Three: Scaling and Governance
Once your pilot has proven its worth, the real work begins: scaling the solution across the wider organization while wrapping it in a rock-solid governance framework. This is where you tackle the long-term challenges head-on—things like data privacy, potential algorithmic bias, and, of course, ironclad compliance with regulations like HIPAA.
Governance isn't just about checking a legal box; it's the foundation of trust. It ensures that as you grow, you do it responsibly, with clear policies for how data is used, how models are validated, and how performance is continuously monitored.
This isn't a niche concern anymore. The global healthcare analytics market is on a trajectory to hit USD 177.18 billion by 2032. And while you might think everything is moving to the cloud, on-premises deployment still commands a 56.8% market share, a testament to how seriously healthcare organizations take data control. This is a complex field, and having an experienced partner to guide you can make all the difference.
Your Questions Answered: Healthcare Decision Enablement
Jumping into healthcare decision enablement brings up a lot of questions. As you start exploring what AI-powered systems can do for your organization, it's completely normal to want clear, practical answers about how it all works, what it's worth, and how to govern it properly.
Here are some of the most common questions we hear from healthcare leaders.
What’s The Difference Between CDS And Decision Enablement?
Think of it this way: traditional Clinical Decision Support (CDS) is just one tool in a much bigger toolbox. CDS typically focuses on giving clinicians alerts and reminders right inside the EHR during a patient visit. It's helpful, but its scope is narrow.
Decision enablement, on the other hand, is the entire strategy. It’s about equipping everyone involved—from the C-suite and financial teams to the patients themselves—with the insights they need to make better choices. It’s not just about a single clinical moment; it’s about making the entire healthcare system smarter.
Where Should Our Organization Start With AI Implementation?
The single best piece of advice? Start small. Find a high-impact problem that isn't overwhelmingly complex. Don't try to solve everything at once.
Look for a specific pain point where you can score a quick, meaningful win. Maybe that’s optimizing OR schedules or predicting no-shows for a single clinic. A focused pilot project like this builds incredible momentum and delivers a tangible ROI you can show to stakeholders.
A solid AI requirements analysis at the outset helps you pick the right problem to solve, paving the way for a successful pilot that earns you the buy-in needed for bigger projects.
How Do We Ensure Our AI Models Are Ethical And Unbiased?
This isn't just important; it's a dealbreaker. Building fair and unbiased AI requires a strong governance framework from the very beginning. Key actions include:
Using diverse and representative data for training your models.
Auditing your algorithms regularly to check for performance drift and bias across different patient groups.
Maintaining transparency so you can always explain how a model reached its recommendation.
Keeping a human in the loop for any critical clinical or operational decision.
This ethical foundation is absolutely essential for building trust. If clinicians and patients see your AI as an unexplainable "black box," they won't use it—no matter how accurate it is.
What Is The Typical ROI For A Decision Enablement Project?
While the ROI depends on the specific use case, it’s almost always significant. For instance, AI models that cut patient readmission rates can save a hospital millions in penalties. Operational gains from AI Automation as a Service can slash labor costs and trim administrative waste. On the clinical side, catching a disease earlier almost always leads to better outcomes and lower long-term costs.
The trick is to define your Key Performance Indicators (KPIs) before you start. You can explore a variety of real-world use cases to see how other organizations have measured success. And to get a sense of what's possible for your team, it's always best to speak with our expert team.
How does decision enablement improve patient safety?
Patient safety is a direct beneficiary of decision enablement. By providing real-time, data-driven alerts, these systems can flag potential issues before they become crises. For example, an AI can predict adverse drug reactions by analyzing a patient's genetic profile and current medications, or it can alert staff to subtle signs of patient deterioration, such as a rising risk of sepsis. This proactive monitoring acts as a crucial safety net, reducing medical errors and improving patient outcomes.
What are the main challenges of implementing a decision enablement system?
The primary challenges include data quality, system integration, and user adoption. High-quality, clean, and accessible data is the foundation, and many organizations struggle with siloed or messy datasets. Integrating AI insights seamlessly into existing workflows (like EHRs) without causing disruption is another major hurdle. Finally, overcoming "alert fatigue" and ensuring clinicians trust and act on the AI-generated recommendations requires careful change management and a user-centric design.
Ready to see what your healthcare data is truly capable of? Ekipa AI provides custom AI strategies and the end-to-end execution to match, turning your biggest challenges into opportunities. Find out how our next-gen platform can help you build a more responsive and intelligent healthcare organization. Get started with your custom AI strategy today.