Your Guide to Modern Healthcare Software Transformation
Discover how modern healthcare software, powered by AI, transforms patient care and operations. Learn to select, implement, and optimize the right solutions.
Long gone are the days when healthcare software was just a digital filing cabinet for patient records. Today, it's a core strategic asset—the engine that modernizes operations, drives better patient outcomes, and keeps the organization financially healthy. In an industry squeezed by rising costs and tangled regulations, the right software isn't just a nice-to-have; it's a competitive necessity.
Why Modern Healthcare Software Is a Strategic Necessity
In the whirlwind of modern medicine, hanging onto outdated, clunky systems is like trying to run a marathon in flip-flops. It’s slow, risky, and guaranteed to cause problems. The conversation has completely shifted. Healthcare software is no longer just another line item on the IT budget; it’s a foundational pillar for clinical excellence and business growth.
This isn't just about swapping paper for pixels. It's a fundamental change in how care is delivered and managed. The right platform can untangle everything from the knot of patient scheduling and billing to the complexities of clinical diagnostics. Investing in smart, agile healthcare software solutions is the first, most critical step in building a resilient, future-ready organization.
The Driving Forces Behind Software Adoption
So, what's pushing providers to finally make the switch? For one, the global healthcare IT market is exploding, projected to hit USD 961.26 billion by 2030. This isn't just a trend; it's a massive shift fueled by the move to the cloud and the power of AI to sharpen clinical decisions. You can dive deeper into the numbers in this research on the growing healthcare IT market on marketsandmarkets.com.
Beyond the big-picture trends, a few critical pressures are forcing the issue:
- Regulatory Headaches: Keeping up with strict rules like HIPAA is nearly impossible with manual systems. Modern software provides the secure, auditable trail that regulators demand.
- The Amazon Effect on Patients: Patients are now consumers who expect slick, digital experiences. They want easy-to-use portals, telehealth appointments on demand, and instant access to their own health data.
- The Burnout Battle: Automation isn't about replacing people; it's about freeing them up. By optimizing workflows and cutting down on administrative grunt work, staff can spend less time on paperwork and more time doing what they do best: caring for patients.
When you start seeing software as a strategic tool instead of a cost center, everything changes. You're not just buying a program; you're building an operational backbone that supports everyone, from the front desk to the operating room. This is how you unlock real efficiency, pave the way for sustainable growth, and ultimately, deliver better care.
Understanding the Healthcare Software Ecosystem
To make smart investments in healthcare software, you first need a clear map of the territory. This isn't about finding a single, magic-bullet product. Instead, it's about understanding a network of specialized tools, each built to solve specific problems for different people in your organization, from the front desk to the operating room.
Thinking this way shifts the conversation from "Which software should we buy?" to "What combination of tools will best serve our patients and our business goals?"
The foundation of nearly every modern clinic is its Electronic Health Record (EHR). Think of the EHR as the central nervous system for patient care—a single, secure place that holds every piece of a patient's medical history. Diagnoses, medications, lab results, treatment plans... it all lives here. It’s the source of truth that every clinical decision relies on.
From that clinical core, other critical systems branch out to manage the operational and financial side of things. Each piece has a distinct job, but they all need to work together.
This diagram shows how a strategic approach puts software at the very heart of the organization, driving everything from day-to-day operations to long-term growth.
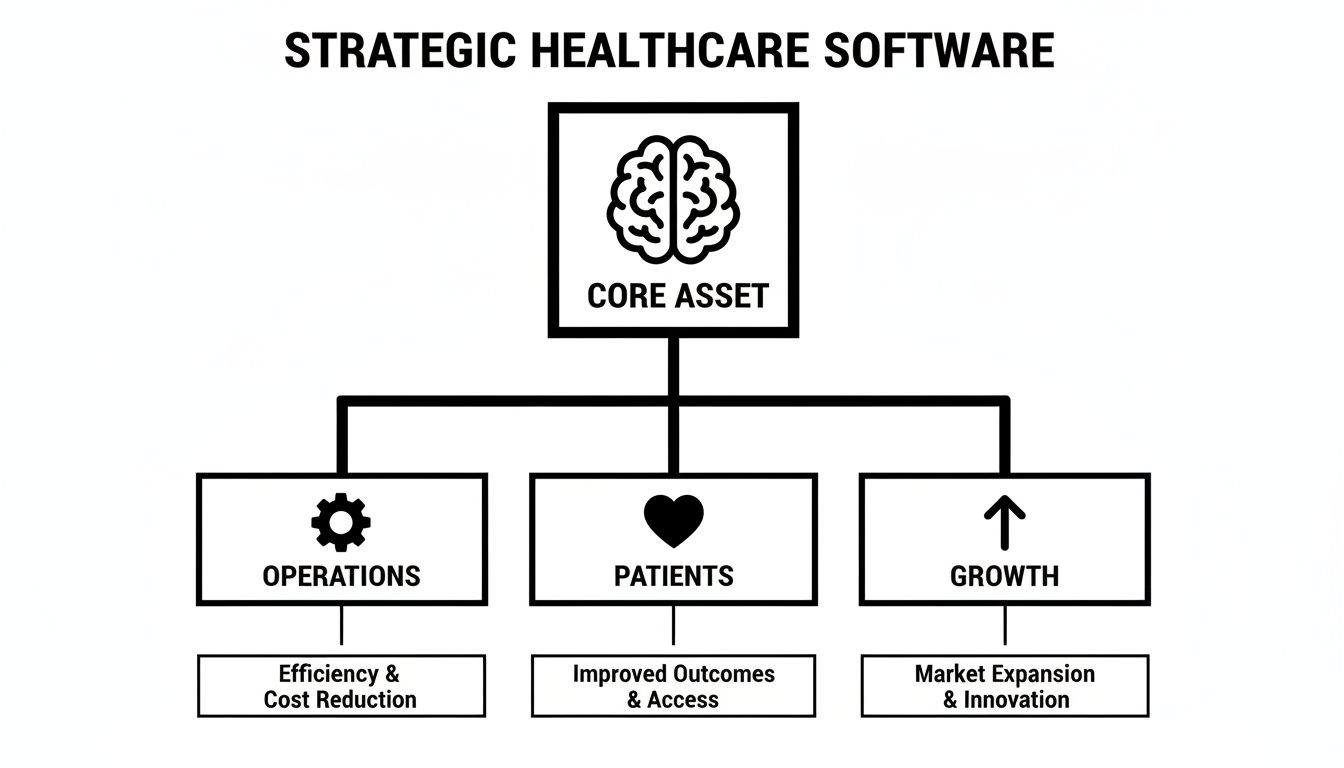
It’s a powerful reminder that software isn’t just an IT expense; it’s the engine that powers a modern healthcare practice.
Key Healthcare Software Categories at a Glance
Getting a handle on the main software categories is the first step to building a tech stack that actually works. Each type addresses a different link in the healthcare chain, and they often need to communicate seamlessly to be effective.
Here's a quick breakdown of the major players you'll encounter.
| Software Category | Core Function | Primary Users | Key Business Benefit |
|---|---|---|---|
| Electronic Health Records (EHR/EMR) | Manages all clinical patient data, including history, diagnoses, and treatments. | Clinicians (doctors, nurses, specialists) | Creates a single source of truth for patient care, improving clinical decisions and safety. |
| Practice Management Systems (PMS) | Handles the administrative and operational side of a clinic. | Front desk staff, office managers, schedulers | Keeps the clinic running smoothly by managing appointments, patient registration, and insurance details. |
| Revenue Cycle Management (RCM) | Manages the entire patient financial lifecycle from start to finish. | Billing specialists, financial administrators | Optimizes financial health by ensuring accurate and timely payment for services rendered. |
| Telehealth Platforms | Enables remote virtual consultations and patient monitoring. | Patients and providers | Expands access to care, improves patient convenience, and creates new revenue streams. |
While these categories cover the essentials, they represent just the starting point for building a truly efficient and interconnected system.
Bridging the Gaps with Custom Solutions
Off-the-shelf software is great for handling standard tasks, but it rarely fits every unique workflow perfectly. This is where the real opportunity lies. By developing tailored solutions, you can fill the critical gaps between your core systems, automating tedious tasks and creating a far more connected and efficient environment. This could involve building internal tooling that integrates disparate systems.
For instance, a custom dashboard could pull data from your EHR and RCM to give leadership a real-time, consolidated view of clinical and financial performance. This is something standard systems often can't do on their own. Similarly, as explored in our guide to Healthcare AI Services, custom AI tools can be built to analyze patient data for predictive insights—a powerful capability not typically found in a standard EHR. For organizations ready to take this step, custom healthcare software development offers a path to truly bespoke solutions.
The ultimate goal is to create a tech ecosystem where every component talks to each other effectively. This integration, whether through standard APIs or custom development, eliminates frustrating data silos and manual workarounds, ensuring your technology works for you—not the other way around.
The Real Impact of AI on Healthcare Software
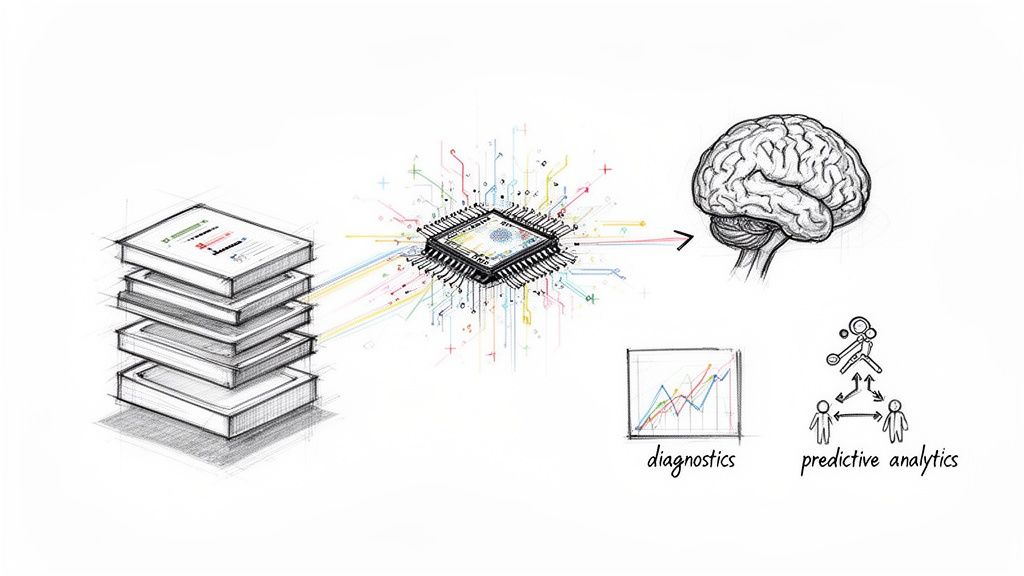
For years, we've thought of healthcare software, like EHRs, as digital filing cabinets—mostly passive systems for storing information. Artificial intelligence is changing that entirely. It's turning those static repositories into active, intelligent partners that can help anticipate needs, flag risks, and guide clinical decisions.
This is a fundamental shift from documentation to prediction. Instead of just showing a patient's history, AI-powered software can model what’s likely to happen next. Think of it as the difference between looking at a paper map of where you've been and using a real-time GPS that reroutes you around a traffic jam before you even see the brake lights.
From Reactive to Proactive Care
Perhaps the most important change AI brings is the move from reactive to proactive care. By crunching massive datasets—patient histories, lab results, genomic data, even public health trends—AI algorithms can spot subtle patterns that are simply invisible to the human eye.
This opens the door to some powerful, real-world applications that are already delivering results:
- Predictive Analytics for Operations: Hospitals can now use AI models to forecast patient admission rates. This helps them optimize staffing and bed allocation, heading off overcrowding and cutting down frustrating wait times.
- Early Disease Detection: In radiology, AI algorithms are becoming a second set of eyes, analyzing MRIs and X-rays to flag potential trouble spots for specialists. In many cases, they can spot the faint signs of disease at its earliest, most treatable stages.
- Personalized Treatment Plans: We're finally moving beyond one-size-fits-all medicine. AI can analyze a patient’s unique genetic makeup, lifestyle, and medical history to recommend the most effective treatment protocols.
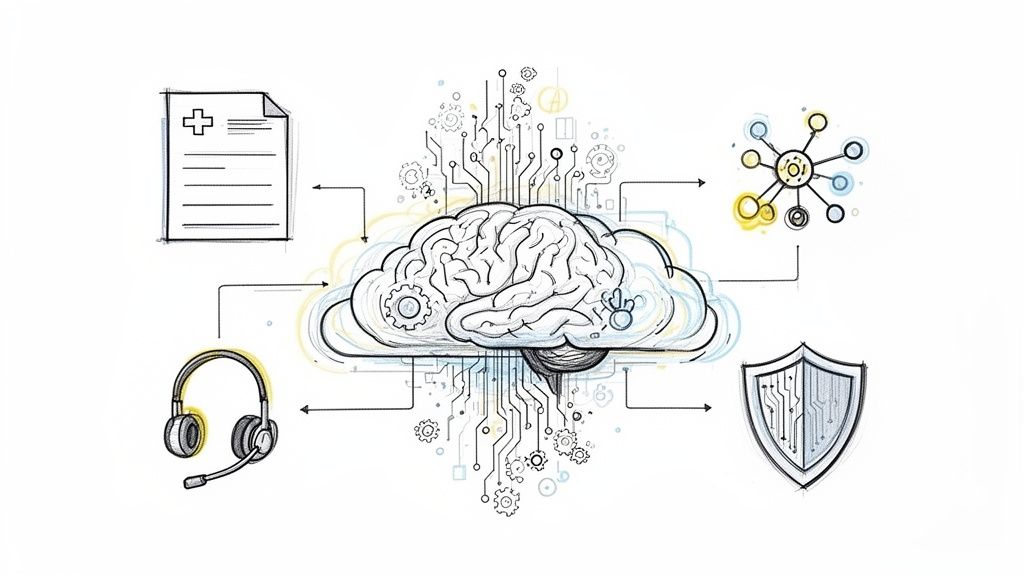
- Administrative Automation: AI is also a workhorse for back-office functions. Many organizations use "AI Automation as a Service" to handle billing and claims processing, which dramatically reduces errors and frees up staff to focus on more complex work.
The point of AI in healthcare software isn't to replace doctors or nurses. It's to supercharge their expertise, giving them better tools to make faster, more informed decisions and to focus their attention where it's truly needed most.
Tangible Applications Reshaping the Industry
It's no surprise that the global healthcare software as a service (SaaS) market is exploding, with projections showing it could hit USD 102.98 billion by 2035. This incredible growth is being fueled by patient portals and AI-enhanced platforms that do far more than just manage data—they actively work to improve outcomes.
For a concrete example, look at how hospitals are using AI to predict which patients are at the highest risk of readmission. By identifying these individuals before they're discharged, care teams can put targeted interventions in place, like follow-up calls or home health visits. This ensures a smoother recovery and helps avoid a costly, stressful return to the hospital.
Of course, getting these advanced technologies right is critical. Integrating them successfully requires a structured plan that ensures the final solution is not only technically sound but also genuinely solves a clinical need and delivers a measurable return. You can also see the broader impact of AI tools for business by looking at tools like a free AI contract generator, which shows how automation is becoming commonplace.
Ultimately, bringing AI into the fold is about building a smarter, more responsive healthcare system. It's about turning raw data into meaningful insights, and then turning those insights into action. This creates a powerful cycle of continuous improvement that benefits everyone involved—patients, providers, and payers.
Navigating Security Compliance and Integration Challenges
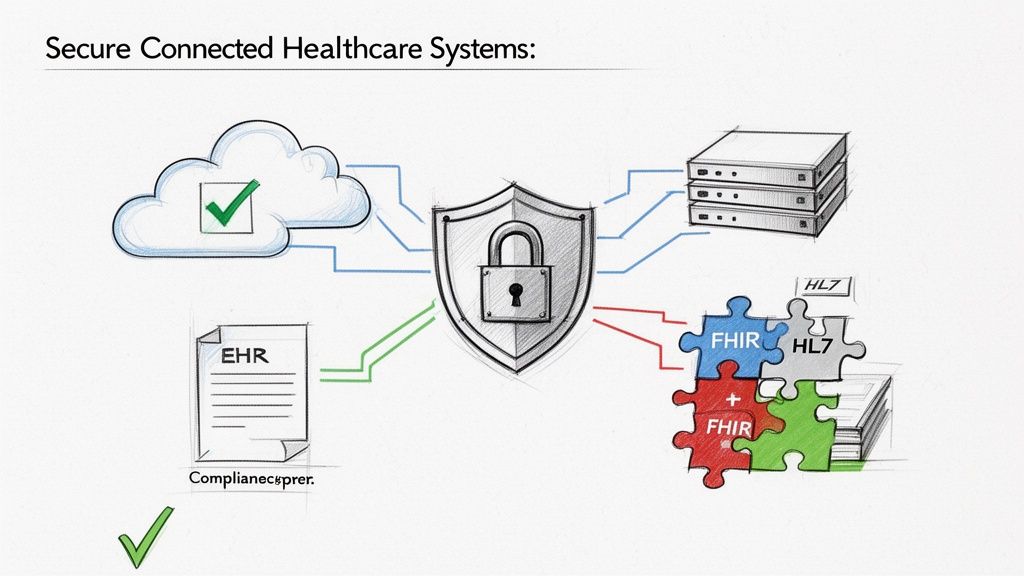
Let's be blunt: even the most impressive healthcare software is a liability if it’s insecure, non-compliant, or can’t talk to your other systems. For any leader in healthcare, these aren't just IT headaches. They're core business risks that directly impact patient safety, legal exposure, and the sanity of your staff. A single data breach or compliance slip-up can trigger a fallout that’s both financially and reputationally devastating.
This is where the conversation shifts from shiny features to the bedrock foundation of your technology. Before you even think about implementing new software, it has to be put through its paces on security and its ability to connect with your existing tech stack. Skipping this step is just asking for expensive fixes down the road, siloed data, and a whole lot of regulatory trouble.
Unpacking the Regulatory Alphabet Soup
Healthcare compliance can feel like a maze of acronyms, but the guiding principles are actually quite simple. These rules exist for one primary reason: to protect sensitive patient information and ensure it’s handled with the utmost care.
You absolutely have to know these two:
- HIPAA (Health Insurance Portability and Accountability Act): This is the big one in the United States. HIPAA sets the national standard for protecting patient health information (PHI), covering everything from who can access data to how it must be encrypted. If a piece of software handles PHI in any way, it must be HIPAA-compliant. No exceptions.
- GDPR (General Data Protection Regulation): While it's a European law, GDPR's reach is global. If your organization handles data for anyone residing in the EU, you're on the hook to comply. It gives people powerful control over their personal data and backs it up with stiff penalties for those who don't play by the rules.
Beyond those, SOC 2 certification has become a key benchmark. It acts as a third-party seal of approval, showing that a vendor has solid systems in place to keep client data secure and private. For many organizations, it's a non-negotiable proof point.
Compliance isn't a one-and-done task you can check off a list. It's a continuous process. Security has to be woven into the fabric of your software and daily operations, from the very first line of code to how your team uses it every day.
The Critical Challenge of System Integration
Your clinic's technology is almost never a single, all-in-one product. It's an ecosystem of specialized tools—your EHR, the billing platform, lab software, and the patient portal all have to work together. The magic that makes this possible is called interoperability, which is just a fancy word for getting different systems to talk to each other and share data smoothly.
When you don't have it, you get data silos. Information gets stuck, forcing your staff into the frustrating and error-prone task of manual data entry. This is precisely why we have industry-wide standards.
- HL7 (Health Level Seven): For years, HL7 has been the go-to standard for swapping clinical and administrative data. Think of it as the established, common language that allows different healthcare applications to communicate.
- FHIR (Fast Healthcare Interoperability Resources): FHIR is the modern evolution of HL7. It's built on web standards, making it far more flexible and efficient for sharing health data across platforms, especially with mobile apps and cloud-based services.
When you're vetting any new healthcare software, checking that it supports modern standards like FHIR isn't just a good idea—it's essential. This ensures the new tool will be a team player in your tech environment, not an isolated island that creates more work for everyone.
A Practical Framework for Choosing and Implementing Software
Choosing and rolling out new healthcare software is a high-stakes decision. Get it right, and you can transform your operations. Get it wrong, and you're looking at wasted money, frustrated staff, and even compromised patient care. This process is far more than just ticking boxes on a feature list; it's a strategic investment that will ripple through your entire organization for years.
A clear, well-thought-out plan turns a high-risk gamble into a predictable project. It’s the best way to make sure the software you choose actually fits your clinical needs and business goals, taking a lot of the risk out of the equation from day one.
Assembling the Right Team
Before you even look at a single vendor, your first job is to build a cross-functional selection committee. This can't just be an IT and executive-level decision. It is absolutely essential to include the people who will use the software every day: your doctors, nurses, front-desk staff, and billing specialists. They’re the ones on the ground who understand the real-world workflows and can spot a potential disaster that leadership might completely miss.
Once the team is in place, their first task is a deep-dive needs assessment. Forget about software for a moment. What problems are you really trying to solve?
- Identify Core Pain Points: Where do things get bogged down right now? Is it the patient scheduling process, the back-and-forth of claims processing, or the time it takes to complete clinical documentation?
- Define Must-Have Outcomes: What does success look like? Be specific. Maybe it’s reducing patient wait times by 15% or slashing billing errors.
- Map Existing Workflows: You need to document how your teams actually get work done, not how they're supposed to. This map becomes the benchmark for evaluating whether a new system will help or hinder your operations.
Nailing this discovery phase is critical. When you have a crystal-clear picture of your needs, grounded in the reality of your end-users, you won't get distracted by flashy features that don’t solve your actual problems.
Evaluating Vendors and Planning the Rollout
With your requirements list in hand, you can finally start talking to vendors. This is where you separate the true partners from the slick salespeople. A great vendor will ask you just as many questions about your workflows as you ask about their software.
You have to look past the sales pitch and get into the nitty-gritty. Insist on live, customized demos that walk through your specific workflows, not some generic canned presentation. And don’t just ask for references—call them. Talk to organizations that are similar to yours in size and specialty to hear their honest, real-world experience with both the software and the vendor’s support team.
A critical mistake is choosing a system that can’t scale with your growth or one that operates in a silo. Prioritize solutions built on modern standards like FHIR that ensure interoperability with your existing and future technology stack.
Planning the implementation is just as important as picking the software itself. A rushed or poorly planned rollout is a recipe for failure. A detailed plan should cover:
- Data Migration Strategy: How are you going to get data out of your old systems and into the new one securely and without errors?
- Phased Rollout Schedule: Are you going to rip the band-aid off all at once (a "big bang" approach), or will you roll it out department by department?
- Comprehensive User Training: This is the one area you can't afford to skimp on. Underestimating the need for training is a common and very costly mistake. You have to budget enough time and resources to get every single user comfortable before the system goes live.
Don’t forget about the non-clinical side of the house. Administrative tools that handle things like the revenue cycle can be completely changed by AI, which can automate claims processing and cut errors by 40-50%. For any leader trying to modernize, these are huge opportunities to reduce operational friction so your teams can focus on patient care. You can find more details in this in-depth market analysis on mordorintelligence.com.
This checklist provides a structured path for navigating this complex process.
Vendor Selection and Implementation Checklist
| Phase | Key Action | Critical Question to Ask |
|---|---|---|
| 1. Discovery & Planning | Assemble a cross-functional team and define core needs. | "Have we included representatives from every department this software will touch?" |
| 2. Requirements Definition | Document must-have features, workflows, and outcomes. | "Does this requirement solve a real, documented pain point?" |
| 3. Vendor Shortlisting | Identify 3-5 potential vendors based on requirements. | "Does this vendor have proven experience with organizations like ours?" |
| 4. In-Depth Evaluation | Conduct custom demos and check references thoroughly. | "Can the vendor show us exactly how their system handles our most critical workflow?" |
| 5. Technical & Security Review | Assess interoperability (e.g., FHIR), security, and compliance. | "How will this system integrate with our existing tech stack, and what is your HIPAA compliance posture?" |
| 6. Contract & Pricing | Negotiate terms, service level agreements (SLAs), and total cost of ownership. | "Are there any hidden fees for support, training, or data migration?" |
| 7. Implementation Planning | Develop a detailed project plan, including data migration and training. | "Who is our dedicated point of contact during the entire implementation process?" |
| 8. Go-Live & Support | Execute the rollout and establish ongoing support protocols. | "What does your 'day one' and long-term support model look like?" |
By following a structured framework like this, you're not just buying a piece of technology. You're making a strategic investment that will pay off in efficiency, staff satisfaction, and better patient outcomes for the long haul. For more detailed insights on managing this process, our guide on the "AI Product Development Workflow" provides a useful model.
Measuring Success and Driving Continuous Improvement
Getting new healthcare software up and running is just the beginning. The real challenge—and opportunity—starts after you go live. Success isn't just about a smooth launch; it’s about proving the software actually improves patient care, makes daily operations easier, and helps your bottom line.
To do that, you need a solid plan for tracking performance. Without clear metrics, you're essentially flying blind, unable to see if your investment is truly paying off or where you can make things better. This is why setting the right Key Performance Indicators (KPIs) is so critical.
Defining Your Key Performance Indicators
To get a real sense of your return on investment (ROI), you have to look beyond the upfront cost. Your KPIs should be a mix of financial, operational, and clinical goals that tie directly back to why you chose the software in the first place. A thorough "AI requirements analysis" done early in the process can give you a strong baseline to measure against.
Think about tracking metrics across these areas:
- Financial KPIs: Are you seeing a drop in billing errors? Have your claim denial rates gone down? Is your revenue cycle moving faster? These numbers tell a clear story about the software's financial impact.
- Operational KPIs: Look for efficiency gains. Are patient wait times shorter? Is there less administrative paperwork bogging down your staff? Can clinicians complete their documentation faster?
- Clinical KPIs: This is where you measure the impact on care. Are patient outcomes improving? Is adherence to treatment plans better? Have you seen a reduction in hospital readmission rates?
Turning Data into a Dynamic Engine for Growth
This kind of data-driven mindset changes your software from a simple tool into a living, breathing part of your growth strategy. The insights you collect should feed right back into how you plan for the future. When you analyze your performance data alongside a detailed "Custom AI Strategy report", you can uncover powerful new ways to optimize and invest.
The real goal here is to build a continuous feedback loop. Performance data should drive your decisions, which in turn leads to constant improvements in both your software and your everyday workflows. This is how you make sure your technology grows with you.
By studying "real-world use cases" and applying those lessons to your own operations, you can spot the next big opportunity for innovation. For any organization that wants to stay ahead of the curve, as we explored in our AI adoption guide, this commitment to measurement isn't just a good idea—it's essential. It's a journey best navigated with a partner, and "our expert team" can help you turn that raw data into a clear path forward.
Got Questions About Healthcare Software? We've Got Answers.
Stepping into the world of healthcare software can feel overwhelming, especially for business and tech leaders. Let's tackle some of the most common questions that come up and clear the air on a few key topics.
What Is the Single Biggest Mistake to Avoid?
It's easy to get dazzled by a long list of features, but the biggest mistake is choosing a system that doesn't fit how your team actually works. A powerful tool that’s clunky and confusing for your staff to use is worse than useless—it leads to poor adoption, frustrating workarounds, and a sea of data entry errors.
The real secret to success is bringing your end-users into the conversation from day one. Look for software that feels intuitive and slots right into your existing workflows. The goal is to make their jobs easier, not to add another layer of complexity.
How Can We Future-Proof Our Software Investment?
Thinking ahead is critical. A smart investment hinges on three things: scalability, interoperability, and a clear path toward AI.
First, go for cloud-native platforms that can grow with you. Second, make sure the system speaks the right language—modern standards like FHIR are non-negotiable for sharing data smoothly with other systems.
Finally, partner with vendors who are already thinking about what's next with artificial intelligence. Using an "AI Strategy consulting tool" can help you map out a forward-thinking plan, ensuring the platform you choose today won't be obsolete tomorrow.
How Long Does a Typical Implementation Take?
There's no single answer here—it really depends on the scale of the project. A small practice might get a new management system up and running in 2-4 months. But a full-scale EHR rollout across a large hospital? That's a much bigger lift, often taking 12-18 months or more.
The timeline gets stretched by things like migrating years of data from old systems, customizing the software to fit your unique needs, and getting everyone trained. We almost always recommend a phased rollout; it’s the best way to manage the chaos and keep daily operations from grinding to a halt.
What's the Real Difference Between EMR and EHR?
These terms get thrown around a lot, often interchangeably, but they aren't the same. Think of an Electronic Medical Record (EMR) as a digital version of an old-school paper chart. It contains the patient's medical history from a single clinic or practice.
An Electronic Health Record (EHR) is the bigger picture. It’s designed to be a complete, shareable story of a patient's health that follows them from their family doctor to a specialist to the hospital. For the kind of coordinated, modern care we're all aiming for, EHRs are the gold standard.
Frequently Asked Questions (FAQ)
What defines modern healthcare software?
Modern healthcare software is more than just a digital record-keeping system. It's a strategic, interconnected ecosystem that uses cloud technology, data analytics, and artificial intelligence to improve patient outcomes, streamline operations, and ensure regulatory compliance. Key features include interoperability (like FHIR), robust security, and user-friendly interfaces for both clinicians and patients.
Why is AI integration crucial for healthcare software today?
AI integration transforms healthcare software from a passive data repository into an active decision-support tool. It enables predictive analytics for disease detection, operational forecasting for resource management, personalization of treatment plans, and automation of administrative tasks. This shift helps providers move from reactive to proactive care, ultimately improving efficiency and patient safety. Our AI strategy consulting can help organizations navigate this transformation.
How can we ensure a new healthcare software system will integrate with our existing tools?
Ensuring integration, or interoperability, is vital. Look for software that adheres to modern industry standards like FHIR (Fast Healthcare Interoperability Resources) and HL7. During the vendor evaluation process, insist on a technical review that confirms the new system’s API capabilities and its proven ability to connect with common systems like EHRs, billing platforms, and lab software.
What is the first step in choosing the right healthcare software?
The first step is internal. Before looking at any vendors, assemble a cross-functional team that includes clinical, administrative, and IT staff. This team should conduct a thorough needs assessment to identify specific pain points in your current workflows and define clear, measurable goals for what the new software must achieve. This foundational work ensures you select a solution that solves real problems for your organization.
Ready to build an AI-powered future for your healthcare organization? Ekipa AI delivers tailored AI strategies and execution support to turn your vision into scalable impact. Our expert team is here to guide you. Discover your AI opportunities today.