Intelligent Scheduling Systems for Hospitals: Boost Efficiency and Care
Discover how intelligent scheduling systems for hospitals use AI to cut costs, boost efficiency, and improve patient care. Get our implementation guide.
Let's get straight to the point—modern hospitals are under incredible pressure. You're dealing with skyrocketing labor costs on one side and persistent staff shortages on the other, all while trying to maintain the highest standards of patient care. It’s a tough balancing act, and it’s precisely why intelligent scheduling systems for hospitals have shifted from a "nice-to-have" luxury to an absolute necessity.
Why Smart Scheduling Is No Longer Optional for Hospitals
If you're still managing complex hospital schedules with spreadsheets or clunky, outdated software, you know the pain. The operational strain is immense. Intelligent scheduling isn't just about booking appointments anymore; it’s a strategic lever for optimizing everything from surgical suite usage to the most intricate staff rosters. These things directly hit your bottom line and, more importantly, your patient outcomes.
At its heart, this advanced approach uses intelligent automation to build schedules that are dynamic, responsive, and even predictive. For any healthcare provider looking to stay competitive and financially sound, this technology is quickly becoming a critical investment.
The Escalating Need for Efficiency
The numbers don't lie. The global market for medical scheduling software was valued at USD 318.5 million in 2023 and is on track to more than double, hitting USD 749.9 million by 2030. This explosive growth isn’t happening in a vacuum; it’s a direct answer to the enormous financial and staffing pressures hospitals face.
Consider this: hospital labor costs shot up by over USD 42.5 billion between 2021 and 2023. At the same time, we're staring down a projected deficit of 100,000 healthcare workers by 2028. In this environment, inefficient scheduling is a massive financial drain.
Every minute a surgeon waits for an OR, or a nurse gets double-booked, it creates a domino effect of delays and piles on overtime costs. Moving to a smarter system isn't about convenience—it's a survival strategy. To see how these AI solutions are being put into practice, you can get more details on our work with AI in healthcare.
The real change here is moving from constantly putting out fires to proactively optimizing your resources. Instead of scrambling to manually fix last-minute changes, an intelligent system can anticipate bottlenecks, balance workloads, and align staff with patient demand—all automatically.
The contrast between old and new methods is stark. I've seen it firsthand in hospitals struggling with outdated processes versus those that have embraced modern, AI-driven tools. It really is a night-and-day difference.
Traditional Scheduling Headaches vs AI-Powered Solutions
To truly appreciate the shift, let's compare the daily struggles of a manual approach with the streamlined reality of an intelligent system.
| Operational Challenge | Traditional Method Impact | Intelligent System Solution |
|---|---|---|
| Staff Roster Gaps | Overworked staff, high burnout rates, and costly last-minute agency hires. | Predicts staffing needs based on patient census data and automatically fills gaps according to credentials and availability. |
| OR Utilization | Idle surgical suites due to poor coordination, leading to lost revenue and longer patient waitlists. | Optimizes surgical schedules by analyzing procedure times, surgeon availability, and equipment needs to maximize throughput. |
| Patient No-Shows | Lost revenue and wasted clinician time from missed appointments. | Sends automated, personalized reminders and offers easy rescheduling options, reducing no-show rates by up to 30%. |
| Emergency Room Overload | Long wait times, patient dissatisfaction, and inefficient patient flow from the ER to inpatient beds. | Forecasts patient influx based on historical trends and community health data, allowing for proactive resource allocation. |
This kind of transformation isn’t a pipe dream; it's entirely achievable with the right strategy and the right technology partner. Making that investment is the first real step toward building a hospital that's more resilient, efficient, and truly centered on patient care.
Creating Your Implementation Blueprint
Making the leap from the idea of intelligent scheduling to a real-world action plan takes a detailed and thoughtful blueprint. A successful rollout isn't just about plugging in new software; it's about weaving that technology into the very fabric of your hospital's most important objectives. This means getting past vague goals like "improving efficiency" and defining exactly what success looks like—in measurable terms—right from the start.
The trick is to think in terms of tangible Key Performance Indicators (KPIs). Instead of a general aim, you need sharp, specific targets. For example, your goal could be to reduce average patient wait times in the emergency department by 15%, boost operating room utilization to 90%, or cut staff overtime expenses by 20% within the first year. These aren't just arbitrary numbers; they are the direct line connecting the technology to core hospital strategies, like improving HCAHPS scores or boosting staff retention.
Defining Your Strategic Goals
Before you even start looking at vendors or algorithms, you need to sit down and be honest about what a "win" looks like for your hospital. What are your biggest headaches right now? Where do you want to be in two years?
A great way to begin is with a foundational AI requirements analysis to get the project's scope right. This process is all about identifying your most pressing scheduling challenges and figuring out how AI-driven tools could solve them. For many hospitals, the sheer volume of data and competing priorities makes this feel like an impossible task. This is where a Custom AI Strategy report can be incredibly valuable, cutting through the noise to help you build a plan that truly fits your unique operational and clinical needs.
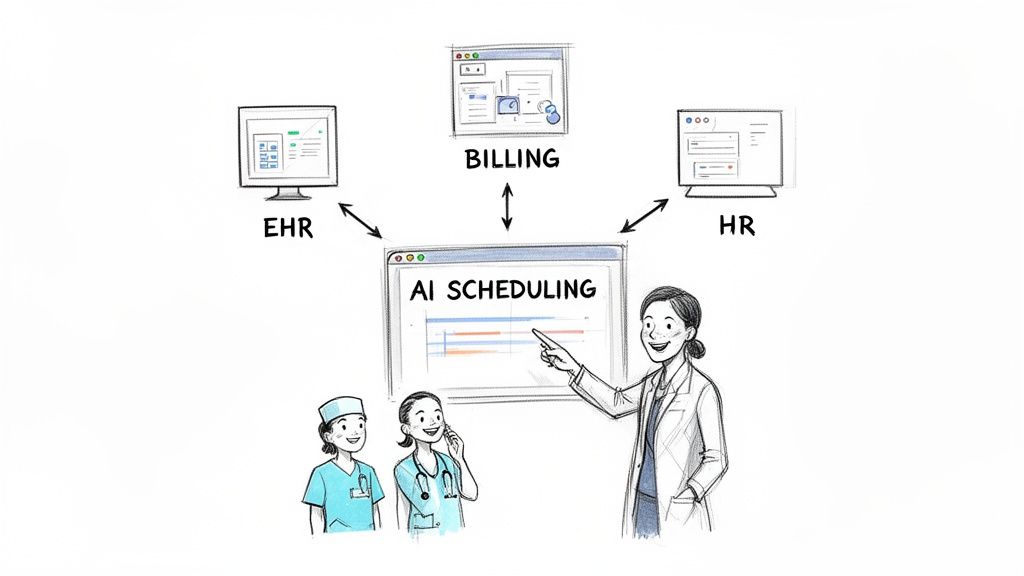
The image below perfectly captures how an intelligent system can turn scheduling chaos into an optimized, predictable process.
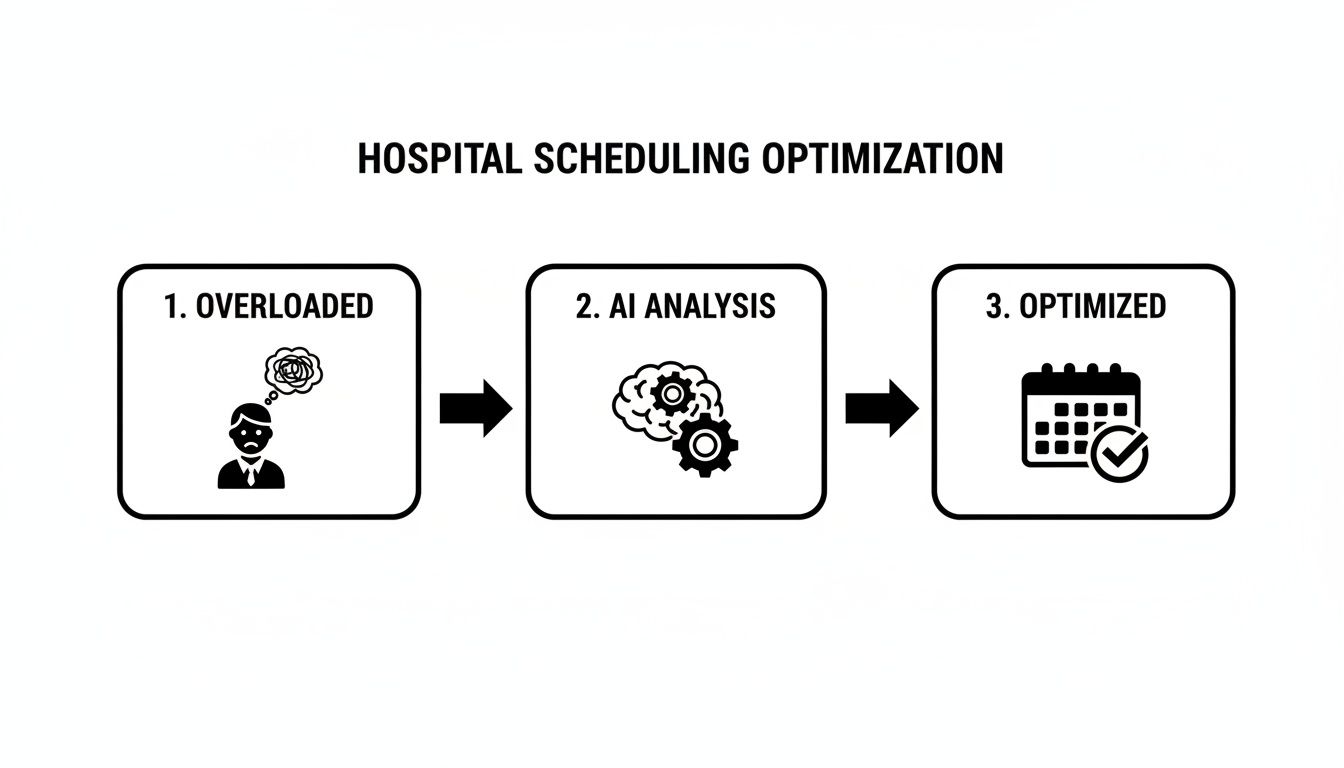
This flow shows the journey from an overwhelmed, manual system to a streamlined one, all powered by focused AI analysis.
Scoping the Project and Setting KPIs
With your big-picture goals in place, it's time to translate them into a manageable project scope with crystal-clear KPIs. My advice? Start small and focused. It’s almost always better to launch a pilot program in a single department—like outpatient imaging or a specific surgical unit—before you even think about a hospital-wide deployment.
Here’s how you can connect your goals to real-world KPIs:
Goal: Improve Patient Access
- KPI: Decrease the average time to the third next available appointment by 25%.
- KPI: Reduce patient no-show rates by 10% using automated reminders.
Goal: Enhance Staff Satisfaction
- KPI: Lower voluntary nurse turnover by 5% annually by offering more predictable schedules.
- KPI: Cut the number of last-minute scheduling changes by 40%.
Goal: Optimize Resource Utilization
- KPI: Increase MRI machine utilization from 70% to 85%.
- KPI: Shave 0.5 days off the average patient length of stay through better discharge planning.
The best implementation blueprints I've seen are living documents. They get revisited and adjusted based on the data and feedback you collect during the pilot. This iterative approach takes a lot of the risk out of the project and helps build momentum for a wider rollout.
This push toward data-driven operations is picking up speed. According to recent hospital AI adoption research, hospital adoption of predictive AI integrated with electronic health records climbed from 66% in 2023 to 71% in 2024.
But there's a catch: system-affiliated hospitals are at 86% adoption, while independent facilities lag far behind at just 37%. This gap shows just how critical a well-defined strategy is. A carefully constructed blueprint isn't just helpful; for many, it's essential for leveling the playing field.
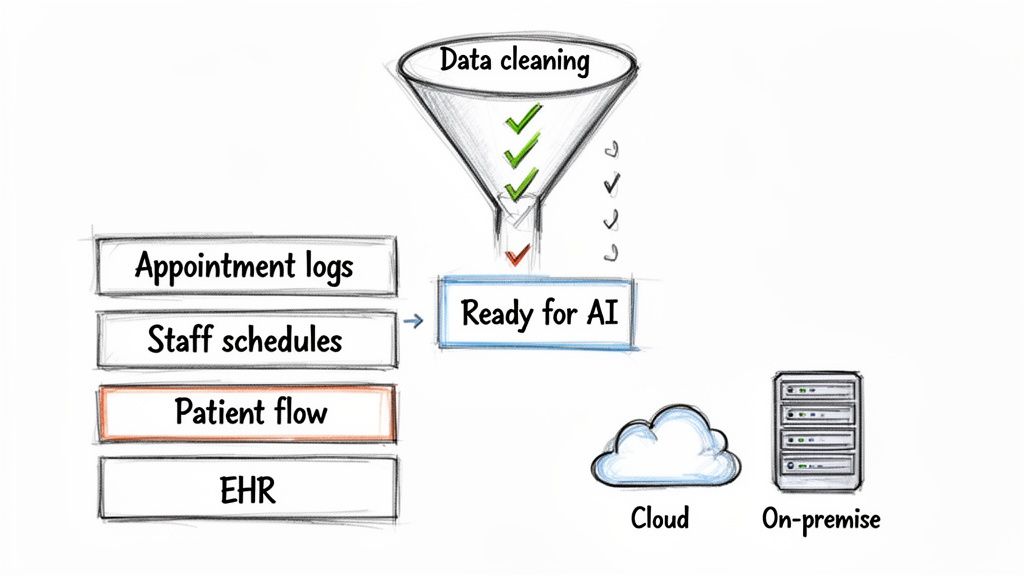
Getting Your Data and Tech Stack Ready
Any intelligent scheduling system, no matter how powerful, is completely dependent on the quality of the data it’s fed. Before you can even think about optimizing patient flow or untangling staff rosters, you have to get your data house in order. This starts with a serious data readiness assessment.
Think of it this way: your data is the fuel for this new scheduling engine. If you pour in dirty, inconsistent fuel, the engine is going to cough, sputter, and eventually stall. In a hospital setting, high-quality data is very specific.
What Good Hospital Data Actually Looks Like
The AI algorithms behind smart scheduling learn from the patterns hidden in your historical data. To make sharp predictions and genuinely useful recommendations, they need clean, complete, and structured information.
Here are the data streams you'll absolutely need to get right:
- Clean Historical Appointment Logs: We're talking detailed records—scheduled appointment times versus actual arrival times, procedure durations, and especially no-show rates. This is how the AI learns true demand.
- Accurate Staff Schedules and Credentials: This is far more than just names on a calendar. The system needs to know staff roles, specific certifications, availability, shift preferences, and historical overtime to build fair, compliant schedules that people actually want to work.
- Reliable Patient Flow Data: You need to map the patient's entire journey, from admission to discharge. This includes wait times at each stop, transfer times between departments, and total length of stay. This data is gold for spotting and fixing bottlenecks.
- Structured EHR Information: Key details from your Electronic Health Record (EHR) system, like patient diagnoses and required procedures, must be accessible and consistently formatted. The AI needs this context to make smart scheduling decisions.
From my experience, the biggest challenges are almost always breaking down data silos between departments and getting everyone to agree on consistent formatting. It's often more of a political challenge than a technical one. Streamlining these kinds of tangled processes is where well-designed internal tooling can make a huge difference.
Choosing Your Technology Architecture
With your data getting into shape, the next big fork in the road is your technology architecture. This usually comes down to one fundamental choice: go with a cloud-based solution or keep it on-premise. Each has its own set of pros and cons, and the right answer depends entirely on your hospital's environment.
A cloud-based system, typically sold as a Software-as-a-Service (SaaS) model, means the vendor handles all the infrastructure, updates, and maintenance. This is great for keeping initial capital costs down and takes a huge load off your internal IT team.
On the other hand, an on-premise solution means you host the software on your hospital's own servers. This gives you total control over your data and security, but it comes with a hefty upfront investment in hardware and requires your IT staff to manage it forever. Given the sensitivity of patient data, prioritizing robust security measures is a must, no matter which path you take.
The cloud versus on-premise debate isn't just about technology; it's a strategic decision. It directly affects your budget, how you allocate IT resources, and your ability to scale in the future. Think carefully about your long-term goals before you commit.
The Build vs. Buy Decision
Finally, you’ll hit the classic "build vs. buy" dilemma. Do you buy an off-the-shelf system from an established vendor, or do you build a custom one from the ground up?
Buying an existing solution is almost always faster and cheaper to get started. These platforms are built on proven models and get regular updates from the vendor. The trade-off? They might not fit your hospital's unique workflows perfectly, and customization can be a real headache.
Building a custom solution gives you complete control and a system that’s a perfect match for your specific operational needs. The downside is a much longer and more expensive development timeline, plus the need for a dedicated team to maintain and support it long-term.
This is where finding a partner with deep expertise in custom healthcare software development can be a game-changer. They can help you weigh the trade-offs and might even suggest a hybrid approach—using a core vendor platform but enhancing it with custom-built modules for the workflows that truly set your hospital apart.
Making It Work: System Integration and Managing the Human Side of Change
You can have the most brilliant AI on the planet, but it's completely useless if your team doesn't embrace it. When you bring an intelligent scheduling system into a hospital, you're not just plugging in new software; you're fundamentally changing how people work. Success hinges on a thoughtful approach that tackles both the technical plumbing and, more importantly, the people.
First, let's talk tech. Your new scheduling tool can't live on an island. It has to talk, and talk fluently, with your existing hospital information systems. This means building solid, two-way connections with your Electronic Health Record (EHR), billing platforms, and Human Resources (HR) software. The goal is a seamless data pipeline: real-time patient updates and staff availability flow into the AI to inform scheduling, while confirmed appointments automatically populate back out to every other system.
The Real Work: Winning Over Your Team
Getting the systems connected is often the straightforward part. The true test is getting your nurses, surgeons, and administrative staff on board—and hopefully, even excited about the change. This is where you have to focus on the "what's in it for me?" for each group.
For nurses, it’s about finally getting fairer, more predictable schedules with fewer last-minute scrambles. For surgeons, it’s about a smarter operating room schedule that cuts down on wasted time between procedures. For the admin team, it means a massive reduction in the hours they sink into juggling phone calls and spreadsheets.
A common pitfall is rolling this out as just another top-down directive. A much better strategy is to position it as a tool that gives your staff more control and frees them from their biggest administrative headaches, letting them get back to patient care.
Our AI Product Development Workflow is built around this human-first philosophy, making sure the technology actually serves the people using it.
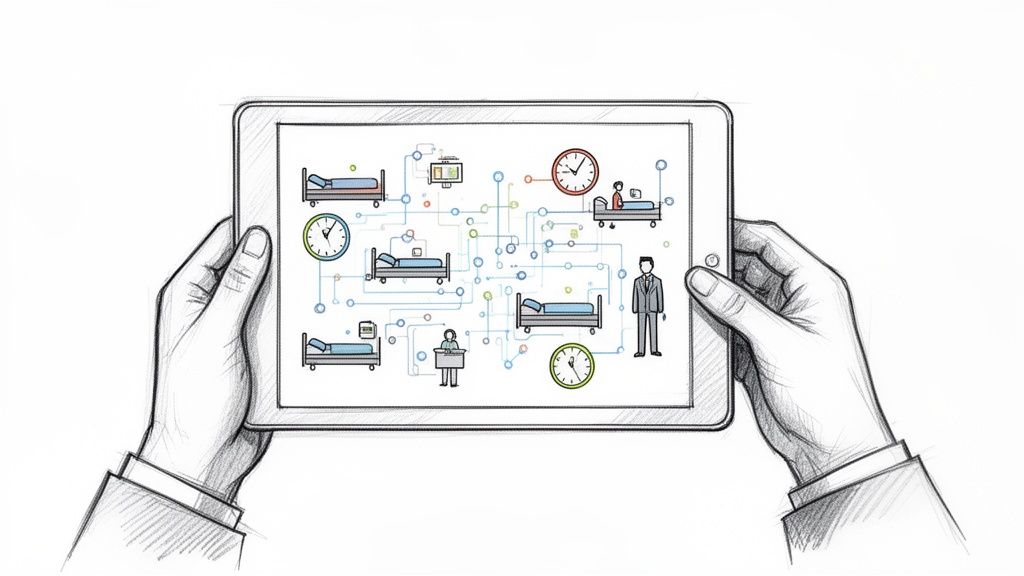
Moving from Whiteboard Chaos to Dashboard Clarity
Think about a typical surgical department. The schedule often lives on a chaotic whiteboard, constantly being erased and rewritten as emergencies pop up and plans change. It’s a recipe for mistakes and a huge source of stress for everyone involved.
Now, imagine swapping that whiteboard for a dynamic AI dashboard. This isn't just a digital display; it actively suggests the most efficient sequence for procedures, flags potential conflicts with equipment, and instantly pings every team member's phone with any updates.
Making that transition happen smoothly requires a clear game plan. Here’s what I’ve seen work best:
- Find Your Champions: In every department, there are always a few people who are excited by new technology. Identify them early and make them your advocates and peer trainers.
- Tailor the Training: A one-size-fits-all training session is a waste of time. Show the nursing staff the features that directly impact their shifts. Show the surgical team how it optimizes their OR time. Make it relevant.
- Open a Feedback Channel: Set up a simple way for everyone to ask questions, report issues, and give feedback during the pilot. When you act on that feedback, you build incredible trust and show that you're actually listening.
This blend of rock-solid technical integration and thoughtful change management is what separates a successful implementation from a failed one. By focusing on turning your skeptics into champions, you ensure the investment you've made in an intelligent scheduling system pays real dividends for your staff and your patients.
Testing the Waters: How to Pilot, Scale, and Measure Real ROI
Theory is great, but it doesn't get you far in a hospital budget meeting. To truly prove the value of an intelligent scheduling system, you have to move past the hypothetical business case and show tangible, real-world wins. This is where a smartly designed pilot program becomes your best friend.
Your mission is to de-risk the investment and build undeniable momentum. It’s about showing, not just telling, how this technology makes life better—for patients, for staff, and for the bottom line. This is a core part of our philosophy in AI strategy consulting; we start with measurable outcomes from day one.
Choosing Your Pilot Department Wisely
Picking the right department for your pilot can be the difference between a stalled project and a hospital-wide success story. You're looking for that perfect blend: a department complex enough to show meaningful results but contained enough that you aren't boiling the ocean. The key is to find a place where scheduling headaches are a well-known, daily frustration.
Think about departments like outpatient imaging or a specific surgical specialty. These are often perfect candidates. Why? Their workflows are heavily structured, they rely on expensive, fixed resources (like an MRI machine or a specific OR), and they produce a ton of data you can actually measure—things like appointment lead times and equipment uptime. A win here is easy to quantify and hard to ignore.
Once you’ve settled on a department, you need to draw a line in the sand. You can't show improvement if you don't know where you started. That means spending at least a month before the pilot kicks off, meticulously gathering baseline data on your key metrics:
- Average patient wait times for an appointment.
- Staff overtime hours directly caused by scheduling chaos.
- The actual utilization rates for key equipment or rooms.
- Patient no-show and last-minute cancellation rates.
A Smart Scaling Strategy
A successful pilot is contagious; it creates a buzz and gets other department heads asking, "When can we have that?" You need to be ready to capitalize on that excitement with a thoughtful scaling strategy. Scaling isn't about flipping a switch and turning it on for everyone overnight. It’s a phased rollout that respects both the technical and the very human challenges of change.
Your scaling plan should map out the answers to a few critical questions:
- Technical Readiness: Can your current servers or cloud setup actually handle the increased demand as you add more departments?
- Integration Roadmap: Who's next in line? What are their unique EHR or HR system integration quirks that you'll need to solve for?
- Ongoing Governance: Who owns this thing long-term? You need a dedicated team to monitor performance, tweak the scheduling rules as things change, and manage system updates. This is a crucial element of our AI Automation as a Service model, which ensures you keep getting value long after the initial launch.
One of the biggest mistakes I see is scaling too fast without actually learning from the pilot. Every new department will have its own unique personality and problems. A phased approach lets you adapt your training and fine-tune your implementation, making each step as successful as the first.
Calculating the True Return on Investment
Measuring the real ROI of a system like this means looking beyond just the obvious cost savings. While those hard numbers are absolutely essential for any business case, the "soft" returns—like less staff burnout and happier patients—are often where the most profound, long-term impact lies. To see what's possible, you can check out our library of real-world use cases.
A complete ROI calculation has to capture both sides of the coin. The framework below is a great starting point for quantifying both the direct financial gains and the equally vital improvements to care quality and staff morale.
Sample ROI Calculation Framework for Intelligent Scheduling
This table gives you a clear template for translating operational improvements into a language that finance leaders understand. It connects the dots between better scheduling and tangible financial outcomes.
| Metric | Calculation Method | Example Annual Impact |
|---|---|---|
| Reduced Staff Overtime | (Avg. Overtime Hours Pre-Pilot - Avg. Overtime Post-Pilot) x Blended Hourly Rate | $150,000 |
| Increased OR Utilization | (Increase in Procedures per Month x Avg. Revenue per Procedure) x 12 Months | $450,000 |
| Lower Patient No-Show Rate | (Reduction in No-Shows x Avg. Revenue per Appointment) x 12 Months | $85,000 |
| Reduced Staff Turnover | (Reduction in Turnover % x Number of Staff) x Avg. Cost to Replace an Employee | $200,000 |
| Higher Patient Satisfaction | (Increase in HCAHPS Scores) linked to higher reimbursement rates and patient loyalty. | Potentially millions in long-term value. |
Looking at ROI this way tells the full story. It positions the investment not just as a cost-cutting tool, but as a strategic asset that drives growth and improves the quality of care. The impact starts in one department but quickly spreads, creating a smarter way of working for the entire organization. This is exactly the kind of strategic shift that our expert team helps hospitals achieve every single day.
Ready to Build a More Efficient Hospital?
Moving to an intelligent scheduling system isn't just a futuristic idea anymore—it's a critical strategic decision. Get it right, and you'll see a direct impact on your operational efficiency, how you use your most valuable resources, and the quality of care you provide. We've walked through the entire roadmap, from setting clear goals to proving the ROI. Now, it's about putting that plan into action.
The first move is always the most important. You need to pinpoint exactly where your scheduling process is breaking down and clearly define what a "win" looks like for your hospital. A well-designed pilot program, concrete KPIs, and a thoughtful change management strategy are what separate successful projects from those that never get off the ground.
Turning Your Plan into a Reality
To make this leap successfully, you need a clear, focused approach. It’s less about a giant, disruptive overhaul and more about smart, sequential steps.
- Map Out Your Strategy: Start with a deep dive into what you actually need. A thorough AI requirements analysis will help you build a practical roadmap instead of just chasing technology.
- Build a Solid Foundation: Take an honest look at your data. Is it clean? Accessible? This assessment will inform the right technology architecture for your hospital's specific environment.
- Bring Your Team on Board: This is absolutely crucial. You need a communication and training plan that addresses concerns head-on, turns your biggest skeptics into advocates, and drives real adoption.
- Test, Measure, and Grow: Launch a small, focused pilot. Meticulously track your KPIs. Once you have the data and proven ROI, you’ll have everything you need to build momentum for a full-scale rollout.
Following this path turns scheduling from a constant headache into a real competitive advantage. The next step is finding a partner who genuinely understands the nuances of healthcare operations and can guide you through each stage.
I've seen it time and again: the most successful implementations aren't just about the tech. They're built on a true partnership—one that starts with a deep understanding of clinical workflows and a shared commitment to delivering real results for both staff and patients.
We believe Ekipa AI is that partner. I invite you to connect with our expert team to talk through your hospital's specific challenges. Let's explore how our AI tools for business can be configured to help you hit your goals. Together, we can build a more efficient future for your hospital.
FAQ: Intelligent Scheduling Systems in Hospitals
How long does an intelligent scheduling system take to implement?
A focused pilot program in a single department typically takes 3-6 months. A full, hospital-wide rollout is a larger project, usually ranging from 9 to 18 months. The timeline depends on factors like data quality, system complexity, and the level of integration required with existing EHR and HR systems.
What is the biggest challenge when implementing these systems?
The primary hurdle is almost always organizational change management, not the technology itself. Staff members are accustomed to existing workflows, so it’s crucial to communicate the benefits clearly—such as fairer schedules, less manual work, and reduced stress. As we explored in our AI adoption guide, involving clinical staff early and providing role-specific training are key to turning potential resistance into enthusiastic adoption.
Can an AI scheduling system integrate with our existing EHR?
Yes, seamless integration with your existing Electronic Health Record (EHR) system is a must-have feature. Modern intelligent scheduling systems use APIs to establish a two-way connection, allowing the AI to pull real-time patient data to inform scheduling decisions and push confirmed appointments back into the patient record. This ensures compatibility with major platforms like Epic, Cerner, and Allscripts.
How does the system ensure scheduling is fair for all staff?
Fairness is achieved through a combination of configurable rules, transparent algorithms, and human oversight. Hospital administrators can define specific constraints within the system—such as limits on consecutive shifts, rules for holiday rotations, and honoring seniority for vacation requests. The AI then optimizes schedules within these predefined guardrails. It's essential to ensure the historical data used for training is free of bias, and a manager should always have the final say to ensure schedules are not just compliant but also compassionate.
What is the typical ROI for a hospital scheduling system?
The ROI comes from both direct cost savings and indirect value. Direct returns include reduced staff overtime (often by 15-20%), increased operating room utilization (boosting revenue-generating procedures), and lower patient no-show rates. Indirect ROI is equally significant and includes reduced staff turnover costs due to higher morale and improved patient satisfaction scores (HCAHPS), which can positively impact reimbursement rates. The combined effect typically results in a payback period of 12-24 months.
Ready to transform your hospital's efficiency and patient care with a smarter approach to scheduling? Ekipa AI delivers tailored AI strategies that turn complex operational challenges into scalable impact. Discover how our AI Strategy consulting tool can help you build a blueprint for success, and connect with our expert team to get started.